Traumatic Diaphragmatic Rupture: A Diagnostic Challenge!
K Vagholkar, S Nair, S Tople
Citation
K Vagholkar, S Nair, S Tople. Traumatic Diaphragmatic Rupture: A Diagnostic Challenge!. The Internet Journal of Thoracic and Cardiovascular Surgery. 2012 Volume 15 Number 2.
Abstract
Traumatic diaphragmatic rupture is usually associated with severe blunt abdominal trauma. It is a marker of the severity of trauma, and is accompanied with serious injuries to other organ systems. Preoperative diagnosis of this condition is a challenge to the surgeon. If missed, it can manifest later in the form of a diaphragmatic hernia- with all of its associated thoracoabdominal morbidity. Delayed repair is associated with increased morbidity and mortality. Hence, diagnosing the condition preoperatively enables immediate repair thus preventing complications. A plain chest x-ray can help in diagnosing this condition. We report here two cases wherein the diagnosis was made preoperatively enabling prompt repair with excellent recovery highlighting the significance of chest x-ray.
Introduction
Traumatic diaphragmatic rupture (TDR) is a rare injury associated with severe blunt abdominal trauma. It is a marker of the severity of the trauma and is associated with rupture of other intra-abdominal organs mainly spleen, liver and bowel. The condition is commonly missed due to presence of other severe injuries, which usually take precedence during the course of management. If missed, it leads to cardio-pulmonary as well as intra-abdominal complications during the post-op period. Hence, if diagnosed pre-operatively, such complications can be prevented. We report here two cases of blunt abdominal trauma with diaphragmatic rupture which were diagnosed pre-operatively by chest x-ray (CXR) along with review of literature pertaining to various diagnostic modalities.
Case Reports
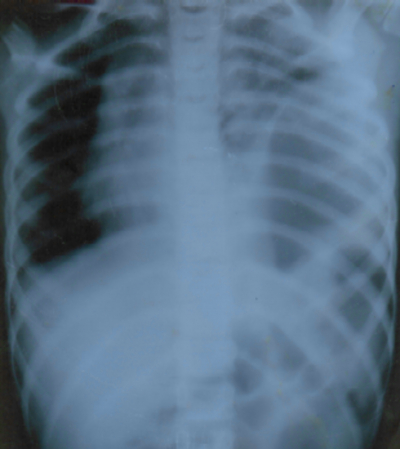
Case 1: This patient in this case was a 9 year old boy who presented with poly-trauma following a vehicular accident. The patient was in profound shock. Physical examination revealed external bruising on anterior abdominal wall in the region of left hypochondrium. There was tenderness and guarding all over the abdomen. Examination of the chest revealed decreased respiratory movements on left side as well as absent breath sounds on left side on auscultation. Primary resuscitation was administered to achieve hemodynamic stability. The CXR revealed herniation of bowel loops in left hemithorax with collapse of the left lung and shift of the mediastinum to the right side (fig. 1). The patient underwent exploratory laparotomy. The left dome of the diaphragm had a rent measuring 10cms. There was herniation of the stomach, bowel loops, and the spleen into the left hemithorax. In addition to this, there was a solitary perforation in the jejunum 2 feet distal to the duodeno-jejunal junction. The abdominal viscera was reduced and reposited back into the abdominal cavity. The base of the left lung was visible but didn’t reveal any tear. The jejunal perforation was closed in two layers after refreshening of the edges. The extent of rent in the diaphragm was clearly delineated. It was sutured with no 1 prolene by way of a continuous suture. An intercostal drain was placed in the left hemi thorax. Peritoneal lavage with normal saline was given, followed by closure of abdominal cavity. The patient required ventilatory support for 48 hours. After extubation, rigorous physiotherapy was instituted. Full lung expansion on left side was achieved in 6 days. Intercostal drain was removed thereafter.
Figure 1
Case 2: This patient was a 12 year old girl who presented with a history of vehicular accidents. The patient had tachycardia but the blood pressure was normal on admission. Externally there were minor abrasions over anterior abdominal wall. Per abdominal examination revealed tenderness and guarding in the left hypochondrium. Examination of the chest revealed decreased air entry in the lower zone of the left lung. CXR revealed an elevated left dome of diaphragm. (fig. 2) The patient underwent exploratory laparotomy. There was large circumferential tear measuring 13cm in length in the left dome of the diaphragm. The upper part of the stomach and spleen had herniated into the left hemithorax. These herniated viscera were reduced into the abdominal cavity. The tear was sutured with continuous suture of no. 1 prolene. Intercostal drain tube was placed in left hemithorax. There was no other intra-abdominal injury. The patient required ventilatory support for 8 hours after surgery. She recovered rapidly after extubation. With good physiotherapy, she achieved good lung expansion in two days following the removal of the intercostal tube.
Discussion
Traumatic diaphragmatic rupture (TDR) is an uncommon injury usually resulting from blunt abdominal trauma. It continues to pose a pre-operative diagnostic challenge to the trauma surgeon. The most common aetiology is blunt abdominal trauma, usually associated with high speed vehicular accidentS or fallS from a height.[1,2] Vehicular accidents are associated with severe frontal impact or impact from the side, leading to thoraco-abdominal injury.[2]
The very presence of this injury is a marker of the severity of impact, necessitating the intense search for other concomitant intra-thoracic and intra-abdominal injuries.[3] Fractured ribs, lung tears and lung contusions are intra-thoracic injuries associated with TDR.[4] Damage to the stomach, small intestine, and spleen with herniation of viscera into left hemithorax causing collapse of lung and mediastinal shift are usually seen in major left sided diaphragmatic tears.[5] Left sided tears usually outnumber right sided tears.[5] This can possibly be attributed to the presence of the liver on the right side, which tends to shield the right hemi-diaphragm. This protective phenomenon is absent on left side, rendering the left hemi-diaphragm more vulnerable to rupture when exposed to very high intra-abdominal pressure.[5] Right sided diaphragmatic ruptures have also been reported.[6,7] These are usually associated with mutilating injuries to the liver (in the case of blunt abdominal trauma) or may follow penetrating injuries on right side.
Bilateral diaphragmatic ruptures have also been reported. [8] These are associated with pericardial rupture. Isolated injury to the left hemi-diaphragm is the most common among all other diaphragmatic injuries. Patients with this injury present with severe shock and prostration, and most of them have concomitant intra-thoracic and intra-abdominal injuries. Emergency management or search for other injuries usually leads to this sort of lesion being overlooked. A variety of imaging modalities are utilised to stage thoraco-abdominal trauma, prior to commencing definitive treatment.
The two cases presented highlight the efficacy of plain CXR in the diagnosis of traumatic diaphragmatic rupture. In both the reported cases, a pre-operative diagnosis of traumatic diaphragmatic rupture could be made. Radiological signs of traumatic diaphragmatic rupture on chest x-ray are elevated dome of diaphragm, herniation of abdominal viscera into the hemi-thorax with shift of mediastinum to the opposite side, and the presence of a Ryle’s tube tip in the left hemithorax above the dome of the diaphragm if x-rayed after insertion of the Ryle’s tube. A plain chest x-ray happens to be the simplest and cheapest investigation in the emergency room setting. The only pre-requisite for radiological investigation in the emergency room setting is achieving haemodynamic stability. [9] Once this is achieved, even a portable x-ray will suffice to make a pre-op diagnosis of traumatic diaphragmatic rupture. This is, by itself, a significant marker of injury severity, pending further radiological imaging in the form of CT-scan, which helps in assessing injuries to other thoracic and abdominal organs thus enabling a complete staging of the traumatic lesions. [8, 10]
CT-scan is an imaging modality which can help in diagnosing traumatic diaphragmatic rupture. Radiological signs on CT are- presence of diaphragmatic discontinuity, herniation of intra-abdominal organs in thoracic cavity, collar or hump sign, dependant viscera sign and abnormally elevated dome of affected hemi-diaphragm. Axial CT-scan has been superceded by sagittal or coronal reconstruction, increasing both the sensitivity and specificity of CT-scan in the diagnosis, dramatic reduction in motion and streak artefact, and significant improvement of the special resolution- especially along z-axis. Helical CT and multi-section CT allow better demonstration of the most subtle signs, such as focal indentation of liver or right sided collar sign.[10]
In haemodynamically stable patients, MRI can also be considered as an imaging modality. MR imaging with breath holding permits good visualization of diaphragmatic abnormality. However, this technique cannot be performed in the emergency room setting. [10]
Once diagnosed, immediate exploration is mandatory. It is good surgical practice to treat other exsanguinating intra-abdominal and intra-thoracic injuries prior to repairing the diaphragm. Adequate assessment with the aim of clearly delineating the site and extent of defect is necessary. If the injury is central, suturing with the help of non-absorbable suture material like prolene will suffice. However, if the injury extends into the periphery, it may be difficult to close the defect. In such circumstances, an intercostal muscle flap will have to be created and used for repairing the defect. Intercostal drain has to be placed in the affected hemi-thorax in order to achieve lung expansion. As repair of hemi-diaphragm will restrict respiratory movements, this can lead to regional atelectasis of the lung. Post-operative ventilatory support is therefore required in most of the cases, as this allows good and controlled expansion of lung in post-operative cases. Once complete expansion is achieved, the intercostal tube can be removed. Often a diaphragmatic injury can be missed; this can give rise to a multitude of complications both intra-thoracic and intra-abdominal. Acquired diaphragmatic hernia is a usual sequel, which leads to compromised ipsilateral lung function, in addition to predisposing the patient to adhesive intestinal obstruction, thus necessitating emergency surgery. A helical CT-scan will help in evaluating the morbid anatomy of the lesion in both the compartments. This serves as a roadmap in deciding which approach to take in repairing the lesion. Majority of these late acquired cases are best approached by the thoracic route. This allows meticulous and careful dissection of herniated contents from lung or pericardium. Morbidity as well as mortality with delayed repair is greater than when repair is performed immediately after diagnosis of the injury in the acute setting. [13]
Conclusion
Traumatic diaphragmatic rupture is an uncommon but lethal sequelae to blunt abdominal injury. Pre-operative diagnosis is pivotal in preventing morbidity and mortality associated with missed rupture. Plain CXR still continues to be the simplest and best of investigations for preoperatively diagnosing this condition, in majority of cases.
Acknowledgements
We would like to thank the Medical Superintendent of Rajawadi Municipal General Hospital, Mumbai, India for allowing us to publish this report.
We would also like to thank Parth K. Vagholkar for his help in typesetting the manuscripts.