The Fontan Procedure And Circulation: The History, Modifications, Complications, And Health Issues
M Sprindzuk
Keywords
cavapulmonary anastomosis, complications, fontan procedure, glenn operation, history, single ventricle, univentricular heart
Citation
M Sprindzuk. The Fontan Procedure And Circulation: The History, Modifications, Complications, And Health Issues. The Internet Journal of Thoracic and Cardiovascular Surgery. 2007 Volume 12 Number 1.
Abstract
The idea of the performance of а surgical shunt, connecting the caval blood flow and the pulmonary artery has allowed to create the several operative methods, which have been applied for 50 years in attempts to improve the clinical status and the quality of life of the single ventricle patients.
The following modifications of the cavapulmonary anastomosis have been described:
1) the original Glenn`s approach - unidirectional end-to-end and end-to-side anastomoses between the pulmonary artery and the superior vena cava;
2) the azygos vein to pulmonary artery connections;
3) the bidirectional - superior and inferior cavapulmonary shunts;
4) the right atrial to the pulmonary circulation connections, with or without valves or patches, including the original Fontan`s and Bjork`s procedures;
5) intaraatrial tunnels with the baffle fenestration in various modifications;
6) connections between the inferior vena cava and the pulmonary circulation via extracardiac conduit, made of synthetic or natural tissues;
7) the direct (without a conduit) anastomoses between inferior vena cavae and the pulmonary artery.
The complications of the cavapulmonary circulation include pleural effusions, low cardiac output, thromboembolism, arrhythmias, protein-losing enteropathy, plastic bronchitis, pancreatitis, liver cirrhosis, nephropathy with microalbuminuria, phrenic nerve injury and diaphragmatic paralysis, neurocognitive deficits, sepsis.
Large-scale clinical trials, experiments are needed to develop the effective clinical strategies and to create the `ideal` cavapulmonary anastomosis.
History of the cavapulmonary circulation
Before the invention and the clinical application of the so-called physiological repair univentricular patients were treated using the aorto-pulmonary shunts or the pulmonary banding. The idea of the creation of the cavapulmonary circulation has been transformed and the modifications of the procedures have been improved. Today this concept is applied as the total cavapulmonary connection – the Fontan operation with extracardiac conduit or the intraatrial tunnel, performed in two steps: first – the bidirectional Glenn procedure or the hemi-Fontan operation, second – the extracardiac Fontan or intraatrial tunnel Fontan, respectively (see table 1). The history of the cavapulmonary anastomosis has been reported in details and with similarities by several authors in monographs "Surgery for Congenital Heart Disease" (Stark, De Leval, Tsang, eds.), J. Kirklin`s and B.Barrat Boyes`s"Cardiac Surgery" and in many others. In this paper, the historical events from available original resources, including Russian monographs are described.
Modifications of the cavapulmonary anastomosis
The following modifications of the cavapulmonary anastomosis have been described:
1) the original Meshalkin-Galankin-Glenn`s approach - unidirectional end to end and end to side anastomoses betweeen pulmonary artery and superior vena cava; 35
2) the azygos and hepatic veins to pulmonary artery connections 36 ;
3) the bidirectional : superior and inferior cavapulmonary shunt 37 ;
4) the right atrial to pulmonary circuit connections with or without valves or patches, including Fontan`s and Bjork`s methods 38 ;
5) intaraatrial tunnels with or without baffle fenestration in various modifications 39 ;
6) the connections between inferior vena cavae and pulmonary circulation via extracardiac conduit, made of synthetic or natural tissues 40 ;
7) the direct (without a conduit) anastomoses between inferior vena cavae and pulmonary artery 41
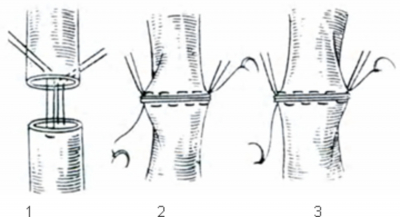
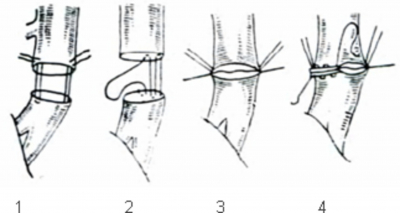
The images of the modern modifications of the Glenn and Fontan procedures are not described in this paper, because there are several published articles and chapters in books on this topic. Figures1-5 show the description of the surgical approaches and the suture techniques, created and performed by Russian surgeons. Today these methods have the historical interest for the cardiovascular surgery professionals and the inventors.
1 – vena cava superior
2 – peripheral end of the right pulmonary artery
3 – cardiac end of the right pulmonary artery
4 – point of the superior venae cavae ligature
1- Π-shaped holding sutures on the anterior and posterior semi-circumference (round) of the anastomosis
2 – connection of the vessels on the medial semi-circumference of the anastomosis
3 - connection of the vessels on the lateral semi-circumference; general view of the completed anastomosis
1 – Π-shaped holding sutures
2 – intimo-intimal suture on the posterior aspects of the vessels
3 – The line of juxtaposition of the intimas after the approximation of the posterior aspects of the vessels via the tension of suture lines
4 – external Π-shaped suture line of the anterior semi-circumference of the anastomosis
Figure 5
1- the line of the pericardial attachment (pericardium has been removed)
2 – the azygos vein
3 – the suture line of the anastomosis
4 – the peripheral end of the right pulmonary artery
5 – the end of the opened pericardium
6 – the cardiac end of the vena cava superior stitched with suturing device
7 – the vena cava superior
1- left vena cava superior
2- left stem of the pulmonary artery
3 – cardiac end of the left pulmonary artery
4 – cardiac end of the left venae cavae superior
Complications of the cavapulmonary anastomosis
The complications of the cavapulmonary circulation include the low cardiac output, pleural effusions, thromboembolism, arrhythmias, protein-losing enteropathy, plastic bronchitis, pancreatitis, liver cirrhosis, nephropathy with microalbuminuria, phrenic nerve injury and diaphragmatic paralysis, neurocognitive deficits, arteriovenous malformations and collaterals, reduced heart rate variability, endothelial dysfunction.
Low cardiac output in Fontan patients
Low cardiac output is the characteristic feature of the cavapulmonary circulation. Newer pharmacologic approaches to the problem include levosymendan 47 and triodthyronine supplement 48 , besides conventional postoperative administration of milrinone and dopamine, epinephrine. Implantation of a pacemaker can positively affect cardiac output in patients with the appropriate indications 49 Ventricular assist devices are used as the bridge to cardiac transplantation 50 Another effective option is external counterpulsation 51
Pleural effusions
Three main mechanisms contribute to the development of persistent pleural effusions after the Fontan procedure: inflammatory, hydrostatic and hormonal. The inflammatory response results mainly from exposure to CPB (cardiopulmonary bypass), causing increased capillary lekeage and subsequent fluid retention. Increased hydrostatic pressure in Fontan circulation results from factors increasing the pulmonary vascular resistance. Lack of atrioventricular synchrony also contributes to this mechanism. The hormonal mechanism involves activation of the rennin-angiotensin system 52 ; Mainwaring et al. 53 , 1995 reported that the data demonstrated that patients who develop effusions following bidirectional Glenn and Fontan procedures have activation of their renin-angiotensin system. Thompson et al. 54 , 2001 reported positive effect of perioperative administration of angiotensin converting enzyme inhibitors on the severity and duration of pleural effusions following bidirectional cavopulmonary anastomosis.
Several studies have evaluated the contribution of preoperative and intraoperative factors to post-Fontan pleural effusions and LOS (length of stay
Gupta et al. 56 , 2004 reported the following risk factors, associated with persistent pleural effusions after extracardiac Fontan: lower preoperative oxygen saturation, presence of postoperative infection, smaller conduit size, and longer duration of cardiopulmonary bypass.
Garofalo et al. 57 , 2006 stated, that ventricular diastolic stiffness predicts perioperative morbidity and duration of pleural effusions after the Fontan operation. Tae-Jin Yun et al. 58 , 2008 reported that low pulmonary vascular compliance is an important risk factor for prolonged pleural effusion drainage after the extracardiac Fontan procedure.
Frommelt et al. 59 , 1995 concluded, that patients with an additional source of pulmonary blood flow after bidirectional cavopulmonary shunt have higher postoperative central venous pressures, have higher oxygen saturations, and are at risk for the late development of a chylothorax.
The performance of the baffle fenestration has been associated with the decreased pleural drainage, the fewer additional procedures and shorter hospital stay (Alphonso et al. 60 , 2005). The management of the persistent postoperative pleural effusion is still considered difficult. Several methods have been reported: fenestration of diaphragm, pleuroperitoneal drainage, low fat diet, parenteral feeding, diuretics, ACE inhibitors, somatostatin (Octreotide) infusions .
Although the exact mechanism of action of Octreotide remains to be clarified, it has been postulated that it could be beneficial to decrease post-Fontan pleural drainage. There are several data, describing its use after the Fontan surgery and other operations 61 (Aleo Lujon et al. 2004; Rimensberger et al., 1998).
Cava et al. 62 , 2005 reported successfull results after the clinical application of the standartized protocol, consisting of diuretics: furosemide 1 mg/kg every 8 hours on postoperative day, when taking liquids, an enteral combination of hydrochlorothiazide and spironolactone 1 mg/kg every 12 hours; afterload reduction using captopril was given at a maximum dose of 1 mg/kg/dose when enteral feeds were initiated; fluid restriction was limited to 80% maintenance; a minimum of 0.5 L of supplemental oxygen by nasal canula was used for its pulmonary vasodilatory effect, regardless of systemic saturation. All patients were on a low-fat diet consisting of 30% of daily calories from fat. Chest tubes were taken out when drainage decreased to 2 ml/kg/day. The duration of chest tube drainage, hospital stay, and the need for pleural sclerosis were significantly reduced, indicating that postoperative management plays an important role in reducing this morbidity.
Arrhythmias
Gradual loss of sinus rhythm is common after the all varieties of the Fontan procedures. Patients with the heterotaxy syndromes, particulary, polysplenia syndrome may also have congenital abnormalities of the sinus node independent of the effects of their surgical procedures (Triedman 63 , 2002). Atrial arrhythmias have been reported between 22% and 50% of patients with an APC Fontan. (Weinstein , Chan 64 , 2005). Alphonso 65 , 2005 reported the following arrhythmias in desending order of appearance: supraventricular tachycardia, atrial flutter, bradyaritmia, atrial fibrillation and nodal rhythm.
A distinctive feature of atrial tachycardias in patients with the Fontan physiology is that they tend to be very organized, regular reentrant arrhythmias. At present, specific factors that appear to be relevant to arrhythmogenesis in the Fontan patient include abnormal size and anatomy of the atrium, myocardial hyperthrophy and fibrosis caused by cyanosis and chronic hemodynamic overload, surgical scarring, and bradycardia-mediated abnormalities of myocardial refractoriness. Frequently identified risk factors for atrial tachycardia include older age at operation and longer follow-up. (Triedman, 2002). Early tachyarrythmia is a predictor for late arrhythmia. Estimated risk factors for atrial flutter include older age at Fontan, longer follow up interval, prior atrial septectomy or pulmonary artery reconstruction, increased symptoms by NYHA class and sinus node dysfunction. Current effective medical therapies for the intraatrial reentrant tachyarrythmia include atrial stabilizing agents such as digoxin, amiodarone, flecanide and propafenone in conjunction with pharmacologic or DC cardioversion (O`Donnel, Lanzberg 66 2002). Electroanatomic mapping is the superior modality for arrhythmia mapping late after the Fontan procedure. Noncontact mapping is limited by a significant reduction in reconstructed electrogram correlation, timing, and amplitude >40 mm from the multielectrode array and cannot accurately define areas of scar and low-voltage endocardium 67
Today it is not yet definitely proven, which Fontan modification is better in terms of reducing the incidence and the severity of the rhythm disorders. The newest modification of the Fontan procedure is the direct inferior vena cava to the pulmonary artery connection may be performed in selected patients with excellent results (McKay 68 , Dearani, 2008). A good option for the patients with double inlet ventricles is the so-called septation procedure - an alternative to physiological repair anatomic approach (Ohuchi et al. 69 , 2008).
Thromboembolism
The blind stump of the main pulmonary artery is the important source of thrombus formation. It should be oversewn as proximally as possible after the excision of the pulmonary valve to minimize this risk (Jonas 70 , 2000; Madan 71 et al., 2002; Kammerad 72 et al., 2004). Either high and low molecular heparins have been used postoperatively with the further treatment with aspirin or warfarin. Alphonso 73 et al., 2005 reported the following indications for warfarin: the arrhythmia, intracardiac thrombus, venous thrombus, pulmonary embolism, the right pulmonary artery stent, embolic cerebrovascular accident. And there has been only one nose bleed related to warfarin in his study. Probably, the combination of aspirin and clopidogrel may be more safe than warfarin and more effective than aspirin alone, but there is a lack of evidence to prove it.
Protein-losing enteropathy
Protein-losing enteropathy (PLE) is a disease with the significant morbidity and mortality seen after the Fontan operation. Mechanisms for the explanation of the pathophysiology of PLE include abnormal mesenteric vascular resistance and inflammation, conditions uniquely present after the Fontan operation. Patients with PLE present with bloating or the abdominal pain, diarrhea, edema, pleural effusion, ascites and distress. Laboratory findings usually include hypoproteinemia, low serum immunoglobulins and calcium levels and low lymphocyte count. The onset may occur from weeks to years after the surgical procedure. In a study by Mertens, this interval ranged from one month to 16 years (mean: 2.7 years). Some cases may present with no diarrhea and with slight hypoalbuminemia, despite the marked reduction in serum immunoglobulin levels and lymphocyte counts, especially of CD4. Subclinical gastrintestinal protein loss may occur with no evidence of the classical clinical findings and with normal serum protein levels. The diagnosis of PLE is confirmed by finding high fecal 1-antitrypsin levels in patients with no other causes of hypoalbuminemia, such as liver disease or malnutrition. The current treatment for PLE is associated with a very high mortality rate. It consists of the diet modification, albumin infusion, diuretics, inotropes, corticosteroids, high- and low-molecular heparin, calcium, spironolactone, gammagloubulin, sildenafil, pacemaker implantation, and surgery: baffle fenestration, intestinal resection and heart transplantation 74 There is an evidence of the therapeutic effect of the octreotide in the patients with PLE with conditions other, than the cavapulmonary circulation 75 , so it could be proposed as the treatment for the single ventricle patients, suffering the complications with the same pathogenesis.
Plastic bronchitis
Plastic bronchitis is a rare complication, in which bronchial casts of the lymphatic origin develop in the tracheobronchial tree and cause the airway obstruction. The main feature of the disease is the expectoration of bronchial casts 76 Treatment modalities include mucolytics and chest physiotherapy and fenestration of the tunnel 77 , aerosolized urokinase 78 or r-TPA 79 , postural drainage, thoracic duct ligation 80 , inhaled heparin 81 , macrolide antibiotics, dornase alfa 82 , oral or inhaled corticosteroids 83 , hydration (Madsen et al., 2005, Ishman et al., 2002) and in the most severe cases bronchoscopy 84 to remove the casts. Stent implantation in the left pulmonary artery 85 , positive effect of sildenafil 86 and bosentan 87 (dual endothelin receptor antagonist which has been used to treat increased pulmonary vascular resistance Votava-Smith et al., 2007). have been reported relatively recently.
Liver dysfunction
Kiesewetter et al. 88 , 2007 reported, that the liver injury, which may be extensive in this patient group, is related to Fontan duration and hepatic vein pressures. According to their opinion and the research data, in the Fontan circulation, central venous pressures are raised by the virtue of the absence of a subpulmonary pump, rendering the systemic and pulmonary circulations in series. The liver, wedged between the raised pressure of the central venous system and the portal venous circulation, superimposes an additional capillary bed and above the pulmonary and intestinal arterial capillary beds. Cardiac output is also frequently depressed, thereby providing the ideal substrate for hepatocyte hypoxia, congestion and stimulation of the fibrotic response. Additionally, during atrial contraction, there is marked flow reversal with the deep intrahepatic reflux with associated hepatic vein distention, causing stromal stretch and compression of adjacent hepatocyte cell plates. Mechanodestruction associated with stretch and compression may be a potent inducer and/or modulator of hepatic fibrosis. Their data suggest that the radiological appearances of the liver on a CT scan may aid in defining liver injury. Hepatic fibrosis and cirrhosis are common findings late in patients reffered for Fontan conversion surgery.
Cardiac cirrhosis with the risk of developing gastro-oesophageal varices and regenerative liver nodules, a precursor to hepatocellular carcinoma, is common in this patient group. Chaloupecky et al. 89 , 2005, documented that almost half the patients after TCPC had laboratory signs of a mild cholestasis. Decreased liver synthesis of procoagulant factors was observed but overall coagulation homeostasis appeared to be in balance in this selected group of patients with a good clinical outcome.
Vasodilator treatment has the potential to reduce the transhepatic and transpulmonary gradient. Recently, sildenafil (phosphodiesterase inhibitor type 5) and bosentan, the non-selective endothelin receptor blocker, have been shown to favourably modulate pulmonary vascular resistance, and in the context of the Fontan circulation, may improve transhepatic perfusion pressures. Their effects on hepatic vascular resistance are unknown. Authors 90 believe that patients, suffering the liver disease are likely to benefit from the creation of a fenestration, but this fact needs prospective evaluation before a general recommendation can be made.
Renal dysfunction
Anne Premchand et al. 91 , 2008 reported the research data, revealing nephropathy with microalbuminuria which was resolved after the prescription of the ACE inhibitor. This unique investigation elucidates the concept of the total protein loss in Fontan patients (via bronchial tree, gastrointestinal and renal systems).
Phrenic nerve injury
Hemidiaphragmatic paralysis after the modified Fontan operation is associated with an increase in early morbidity. Care should be taken to avoid the injury to the phrenic nerve. Early diaphragm plication may be favorable to optimize the Fontan circuit in patients with diaphragmatic paralysis 92
Neurologic and behavioral problems and general health.
In children with univentricular heart, intellectual and neurologic deficits, the syncope, the problems with learning are common. In the multiple linear regression model (Sarajuuri et al., 2007), diuresis the third day after the primary operation and cardiopulmonary bypass time in the bidirectional Glenn operation correlated significantly with the primary outcome of full-scale IQ, which was reported the lowest in HLHS patients. 93
Systemic inflammatory response syndrome and septic schock
Cases of septic shock after the operations of physiological repair are reported rather rare, in single accidents. Both fungal and bacterial etiology of the systemic inflammatory response after the Fontan procedure occurs 94 It is known, that such complications as the protein-losing enteropathy, plastic bronchitis and prolonged pleural effusions are associated with the development of the acquired immunodeficiency 95 , increasing the vulnerability of the patient to the invading antigens. Probably, splenic dysfunction in heterotaxy patients may contribute to the problem.
Endothelial dysfunction
Binotto et al. 96 , 2005 concluded that the vascular endothelium plays a central role in the control of coagulation and fibrinolysis. The data suggest that patients with the Fontan circulation may have endothelial dysfunction, as indicated by raised levels of von Willebrand factor. Fibrinolysis seems to be relatively preserved, as suggested by the appropriate response to the venous occlusion.
Endothelial dysfunction is more prevalent in the Fontan patients, compared with the healthy controls, and the previous hypoxia is an independent factor. Although it is not statistically significant, those patients on treatment with ACE seem to have better endothelial function (Jin 97 et al., 2007).
In case of Fontan operation failure, the histological modifications are subtle with a muscular extension of the distal pulmonary arterioles wall. Conversely, a marked increase of NO synthase and VEGF expression is observed which can witness of an endothelial dysfunction. (Levy et al. 98 , 2004).
In Fontan patients, diminished exercise capacity was related to a reduced blood flow supply and an attenuated post-exercise oxygen resaturation of the working skeletal muscle, which also was related to the impaired endothelium-dependent vasodilation (Inai 99 , 2004).
Morgan et al. 100 , 1998, have found the higher shear stress, acting on the wall of the vessels in the patients, having a bicaval tunnel, which may alter the endothelial function and affect the longevity of the repair.
Altered levels of endothelial markers in the plasma, in the presence of normal levels of d-dimer, suggest that endothelial dysfunction may precede the occurrence of intravascular coagulation and thrombosis in patients with functionally univentricular physiology. These observations may have therapeutical implications (Binotto et al. 101 , 2007).
Arteriovenous malformations and collaterals
In children with univentricular circulation after Glenn or Fontan operations, the increased central venous pressure may induce recanalization of embryologically preformed and obliterated vessels. Finally, such venous collaterals can result in systemic desaturation and reduction in ventricular function (Usta 102 et al., 2008).
Aorto-pulmonary collaterals are among etiology of pulmonary hemorrhage and hemoptysis together with pulmonary hypertension, pulmonary venous congestion, pulmonary arteriovenous malformations, and dilated bronchial arteries (Deisenberg 103 , 2005). Bleeding gastric varix due to the development of collaterals from high-pressure systemic vein to low-pressure portal vein can be a late complication of total cavopulmonary shunt . (Furuse 104 et al., 1993).
Because the hepatic venous return in left atrial isomerism patients is not directed to the lungs, the portal venous pressure is lower than the systemic venous pressure. Thus, there would seem to be a risk for the late development of collaterals and fistulous communications between the systemic venous and hepatic venous system leading to progressive systemic desaturation (Usta 105 et al., 2008).
The prevalence of collaterals is considered as a common complication after cavopulmonary connection and varies between 20.2% to 31% of the patients. A late manifestation is rare. While Fontan completion is one choice of treatment, the other therapeutical option to eliminate such collaterals consists of percutaneous coil embolisation. Non-cardiac surgery as the favoured therapeutical choice for occlusion of such massive venous collaterals may be beneficial in selected patients with impaired ventricular function and rather complex collateral anatomy, who otherwise were high-risk Fontan patients (Vettukattil et al. 106 , 2000)
Detailed angiographic evaluation on a routine basis allows identification of the vascular sites of origin of aortopulmonary collateral vessels and systemic venous collaterals potentially developing during long-term follow-up. Transcatheter interventions, including fenestration occlusion and occlusion of venous collaterals and aortopulmonary collaterals should be performed to maintain and improve the Fontan circulation in clinically symptomatic and asymptomatic patients. During long-term follow-up after Fontan-type operations, a regular postoperative cardiac catheterization protocol is recommended (Kaulitz 107 et al. 2002, Stumper 108 et al., 1995).
Reduced heart rate variability
Autonomic nervous control of the heart can be studied by analysing variability in heart rate. In patients with the Fontan circulation, routine ambulatory electrocardiographic monitoring including analysis of variability in heart rate, detects over time a progressive sympatovagal imbalance and reduction of HRV (Rydberg 109 et al., 2005).
Elevated neurohumoral activity and an abnormal cardiopulmonary response to exercise are well-established characteristics in patients after the Fontan operation. Angiotensin-converting enzyme inhibitor administration does not change this abnormality (Ohuchi et al., 2002) 110
Surgery on the caval veins and the atria alters the intracardiac ganglia that are abundant at the cavo-atrial junction and in the myocardium of the right atrium. Abnormalities of HRV in Fontan patients may act as a co-factor in the initiation of arrhythmia in these patients (Butera 111 et al., 1999).
Pancreatitis
The impaired ventricular relaxation, compression and obstruction of conduit are associated with the occurence of the severe fatal pancreatitis. Toxicities of drugs and the adverse effects of cardiopulmonary bypass contribute to the pathogenesis of this devastating disease 112
Conclusion
Future clinical trials will show the advantages and the disadvantages of the modern modifications of the cavapulmonary anastomosis and the effects of the therapeutic strategies. The great progress has been done to improve the treatment of the single ventricle patients. I hope that this brief review article will help to receive more useful knowledge to treat the suffering patients.