Gastro-Intestinal Stromal Tumor (GIST) of the Ampulla of Vater: Report of Two Cases
D Mohapatra, T Mishra, A Dash, M Ibrarullah, P Devi
Keywords
gist, hematemesis, periampullary tumor
Citation
D Mohapatra, T Mishra, A Dash, M Ibrarullah, P Devi. Gastro-Intestinal Stromal Tumor (GIST) of the Ampulla of Vater: Report of Two Cases. The Internet Journal of Surgery. 2013 Volume 29 Number 1.
Abstract
Gastrointestinal stromal tumor (GIST) of the ampulla of Vater is extremely rare. A literature search yielded only 10 such reported cases till date. We present two cases of ampullary GIST, one benign and another malignant. The benign tumor presented with massive hematemesis and melena. The malignant tumor presented with obstructive jaundice. Both cases were successfully resected.
Introduction
Gastrointestinal stromal tumor (GIST) was first reported in 1983 by Mazur and Clark to describe nonepithelial tumors of the gastrointestinal (GI) tract that lacked the ultrastructural features of smooth muscle cells as well as the immunohistochemical characteristics of Schwann cells1. GIST represent only 0.2-3 % of GI malignancies having an estimated incidence of 10-20 /million2, 3. Stomach (40–60%) is the most common location of GIST followed by small intestine (30–40%), colo-rectum (10-15%) and duodenum (3–5%)4. Involvement of the ampulla of Vater is extremely uncommon. The available publications on this entity are in the form of anecdotal case reports only. We report two patients with ampullary GIST that was managed by us.
Case 1
A 45-year-old female was admitted with hematemesis and melena for two days. She had a similar attack 45 days back for which she was transfused four units of blood. Upper GI endoscopy during the present admission showed fresh blood in stomach and duodenum. On side-viewing endoscopy, the ampulla of Vater appeared bulky with an ulcer on its surface (Fig. 1).
Biopsy of the ulcer was inconclusive. Her hemoglobin was 5g/dl. Other hematological and biochemical parameters were within normal range. During the present hospitalization she had another episode of bleeding necessitating an emergency laparotomy. The ampulla felt nodular from outside. The rest of the abdominal viscera appeared normal. The patient was subjected to pylorus-preserving pancreaticoduodenectmy (PPPD). The resected specimen showed a nodular and ulcerated ampulla with a visible vessel at its center (Fig. 2).
Figure 2
The patient made an uneventful recovery except for a pancreatic anastomotic leak that was managed conservatively. Histopathology of the tumor was consistent with benign ampullary GIST (mitotic figure of 5/50 HPF). Immunohistochemical study of the tumor was positive for CD 34, c-kit and SMA, negative for Desmin and S -100. The patient remained healthy at follow-up of 18 months.
Case 2
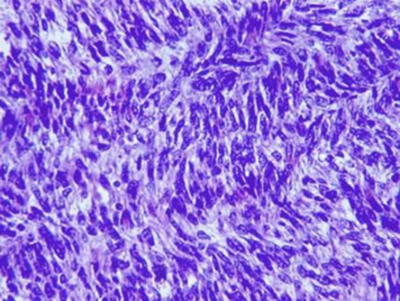
A 52-year-old male was admitted with complains of painless, progressive jaundice, and anemia of one and half month duration. His blood investigations revealed Hb of 7. 8 g/dl, serum total and direct bilirubin of 6.3 g/dl and 5 g/dl, respectively. Serum alkaline phosphate was 1800 mg/dl, SGOT 37 mg/dl and SGPT 46 mg/dl. Upper GI endoscopy showed an ampullary tumor and biopsy was inconclusive. Ultrasonography (USG) showed distended gall bladder, dilated intrahepatic biliary radicles (IHBR) and dilated (1 cm) common bile duct (CBD) with an abrupt cut-off at the distal end. Contrast-enhanced CT scan of the abdomen showed a hyperdense 4 x 3 cm periampullary lesion with dilatation of CBD and IHBR. A clinical diagnosis of periampullary carcinoma was made and the patient was subjected to PPPD. In the post-operative period the patient had prolonged gastric ileus that was managed conservatively. Histopathology of the tumor was consistent with malignant GIST (Fig. 3) with a mitosis count of 20/50 HPF.
Figure 3
The cut margin of specimen and lymph nodes were free of tumor. The patient was discharged on the 25 th postoperative day. In a follow-up of 30 months, he has remained disease-free and in good health.
Discussion
GIST is thought to arise from the interstitial cells of Cajal (ICC), a component of the intestinal autonomic nervous system.5 In 1998, Hirota and colleagues demonstrated gain-of-function mutations of the KIT proto-oncogene in the vast majority of GISTs.6 GISTs are now identified by the near-universal expression of the CD117 antigen (95%) which is characteristic of most GISTs. Expression of CD-34 has been reported in 60-80% of GISTs. Approximately 7% of GISTs have gain-of-function mutations in the PDGFRA tyrosine kinase receptor.7
After extensive review of literature and online search, we could find only 10 reported cases of the GIST of the ampulla of Vater8-17. The tumor is commonly encountered in the fifth and sixth decades of life without any preference for sex, race or ethnicity. Ampullary GIST may present with weight loss, nausea, melena, anemia and jaundice. Though GIST almost never metastasizes to regional lymph nodes, there has been one documented case of ampullary GIST presenting with multiple liver and lymph node metastasis14. Tumors giving rise to metastases are generally more than 5 cm in diameter and have a high mitotic index (>10 mitoses/HPF). However, up to 20% of small GISTs (<5 cm) can also exhibit metastatic behavior. The recognition that all GISTs have some malignant potential, has now led to their classification as either low, intermediate, or high-risk based upon tumor size and mitotic count.3, 18
A preoperative diagnosis of GIST may affect the mode of treatment offered to the patient8-17. This has ranged from local resection (3 patients) to Whipple’s procedure (6 patients); one patient died due to metastasis before any surgery was undertaken. An accurate preoperative diagnosis, however, may be extremely challenging. The reason being (i) presenting as a mass in the ampullary region it mimics periampullary carcinoma, (ii) preoperative endoscopic ultrasonography, though it has been reported to be highly successful in both documentation and biopsy confirmation, is still not readily available or expertise may not be present everywhere. One of the cases reported here underwent pancreaticoduodenectmy with a preoperative clinical diagnosis of ampullary carcinoma. The second patient underwent an emergency resection for massive bleeding before biopsy confirmation could be obtained. Use of Imatinib in duodenal GIST preoperatively to control bleeding has been reported19 but it is still very early to speculate on its use in ampullary GIST. Given all considerations, pancreaticoduodenectomy is probably an appropriate mode of treatment for ampullary GIST.17, 20