Primary Colon Lymphoma: A Rare Cause of Small-Bowel Obstruction
S Cheddie, B Singh
Keywords
chemotherapy, colorectal surgery, extranodal lymphoma, large intestine, non-hodgkin lymphoma
Citation
S Cheddie, B Singh. Primary Colon Lymphoma: A Rare Cause of Small-Bowel Obstruction. The Internet Journal of Surgery. 2013 Volume 29 Number 1.
Abstract
Primary colonic lymphoma is rare and accounts for 0.2-1.2% of colonic malignancies. The non-Hodgkin B-cell variety is the most common type with a predilection for the ileocecal region. The disease may mimic adenocarcinoma of the colon and gastrointestinal tuberculosis. Intestinal obstruction rarely occurs; however, spontaneous perforation of the colon is reported in up to 45% of cases. Diagnostic work-up includes colonoscopy, contrast enemas, CT and PET-CT scans; however, these tests are often non-specific and the diagnosis is commonly made on histopathology of hemicolectomy specimens. Surgery is the mainstay of therapy while cytotoxic chemotherapy (CHOP regime) is routinely employed in the adjuvant setting. Prognosis depends on the histological grade and stage of the disease at presentation.
Introduction
Primary colon lymphoma is a rare cause of gastro-intestinal malignancy accounting for 0.2% to 1.2% of colon malignancies. The gastro-intestinal tract is a common site of extra-nodal lymphoma; the non-Hodgkin type (NHL) being the commonest variety. The stomach is the most common site of gastrointestinal lymphoma (50-60%) followed by the small intestine (20-30%) and the colon and rectum (10-20%)[1]. We present a rare case of primary cecal lymphoma with impending small-bowel obstruction.
Case Presentation
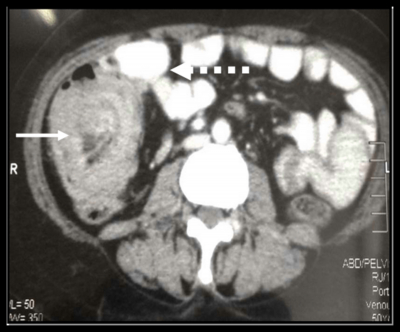
A 55-year-old African female presented with a 3-month history of weight loss and right iliac fossa pain. She had no constitutional symptoms of tuberculosis and no associated history of altered bowel habits or rectal bleeding. A physical examination revealed temporal wasting and pallor with no evidence of lymphadenopathy. Abdominal examination revealed abdominal distension with a palpable, firm, mobile right iliac fossa mass. Biochemistry revealed a haemoglobin of 8.7g/dL and an albumin of 25g/L. She was HIV negative with an ESR of 35mm/h. A CT scan of the abdomen revealed a large heterogenous annular mass arising from the cecum with luminal narrowing and dilatation of the small intestine (fig. 1). Localised mesenteric lymphadenopathy was present with no evidence of distant metastatic disease. In view of the impending small bowel obstruction, a right hemicolectomy with primary end-to-end anastomosis was done (fig. 2). The histopathology revealed a diffuse high-grade B-cell lymphoma with immunohistochemistry showing CD20-positivity. The post-operative course was uneventful and the patient was referred to a hematologist for further management.
Figure 1
Discussion
The colon remains an uncommon site for extranodal NHL. The sites most commonly involved are the ileocecal region (47%), cecum (29%), sigmoid (18%) and rectum (6%). The reason for the predilection for the ileocecal region is unknown; however, it is postulated that the proliferation of lymphoid tissue occurs in the Peyer’s patches in this area. The disease occurs more commonly in adults with predominance in males[1].
Primary lymphomas of the colon may be diffuse (lymphomatosis coli) or localized to a single anatomical region; the B-cell variety being the most common subtype in Western countries. In more than half of patients, the tumour presents with a bulky abdominal mass (>5cm) and non- specific symptoms. Intestinal obstruction is uncommon due to the pliable nature of the tumor and the absence of a desmoplastic response[2].
A pre-operative tissue diagnosis may be obtained by colonoscopy in the non-emergency setting; however, adequate tissue specimens to allow for full immunohistochemical staining are not always possible. CT scanning of the abdomen may show polypoidal, annular, ulcerating and nodular lesions with associated intra-abdominal lymphadenopathy. Distinctive features of primary colon lymphoma from adenocarcinoma are as follows: spread to the terminal ileum, preservation of fat planes, an absence of adjacent organ invasion, and a high incidence of perforation due to the lack of a desmoplastic reaction[3]. The features are non-specific and may mimic abdominal tuberculosis. Contrast studies demonstrate diffuse or localized lesions that may appear ulcerating or polypoidal. The PET-CT scan has been shown to have a greater sensitivity (97%) and specificity (100%) for staging of NHL and is superior to conventional CT scan in detecting recurrence and monitoring the response to chemotherapy[4].
Surgery remains the mainstay of therapy for treating colon lymphoma[2]. Due to the high risk of spontaneous perforation (45%), a hemicolectomy is advised to obviate this complication. Surgery alone may be adequate therapy for low-grade NHL limited to the submucosa[1]. The CHOP regime (cyclophosphamide, doxorubicin, vincristine and prednisone) is administered in the adjuvant setting. An improvement in median survival from 36 to 53 months has been reported in patients who underwent adjuvant chemotherapy[5]. Several prospective trials have shown that adding rituximab (monoclonal antibody to CD20) to the standard CHOP regimen (R-CHOP) resulted in higher response rates and better progression-free, event-free, disease-free and overall survival[6]. External beam radiation is most commonly used for regional adjuvant therapy to obtain local control after incomplete resection.
Conclusion
Primary colon lymphomas are rare. A high index of suspicion with appropriate diagnostic investigations is necessary to make a pre-operative diagnosis; however, the diagnosis is often made post-operatively on formal histopathology. Surgery remains the mainstay of therapy for colon lymphoma due to the high risk of spontaneous colonic perforation and cytotoxic chemotherapy (CHOP regimen) is routinely used in the adjuvant setting. Due to the rarity of this condition combined with a paucity of prospective randomized evidence, treatment should be individualized according to the patient profile and clinical presentation.