Laparoscopic Management of Varicocele – A Hospital based study
A Tarun, J Veenu, K Dhanesh, P Sanjay
Keywords
laparoscopic varicocelectomy, mass ligation, varicocele
Citation
A Tarun, J Veenu, K Dhanesh, P Sanjay. Laparoscopic Management of Varicocele – A Hospital based study. The Internet Journal of Surgery. 2009 Volume 23 Number 2.
Abstract
Background/Purpose: The authors present their experience with laparoscopic ligation of varicoceles (LVL) with and without mass ligation.Methods: Over a period of 3 years, 76 patients underwent laparoscopic treatment of unilateral varicoceles (age range, 9 to 36 years); 35 underwent ligation of veins alone and 41 underwent ligation of testicular veins and artery.Results: The average operation time for the artery-preserved and the artery-ligated group was 36 (range 14 to 50) minutes and 19 (range 12 to 26) minutes, respectively, and the average hospital stay was 26hrs and 21 hrs, respectively. There were no technical failures. Complications were less in the mass-ligation than in the artery-preserved group. At an average follow-up of 24 months (range 6 to 30), all patients were asymptomatic and had marked reduction in the size of the varicoceles.Conclusion: LVL is safe, effective, less time consuming and has excellent post-operative results. LVL should preferably be done with en-bloc mass ligation with an attempt to spare lymphatics.
Introduction
Varicocele is an abnormal dilatation of the veins of the pampiniform plexus. It occurs in 6% of children at age of ten, 13% of adolescents and 15% of males in the general population. However, varicocele has been observed in 35% of men with primary infertility and up to 80% of men with secondary infertility. The detrimental effect of varicocele on spermatogenesis in the subfertile male is manifested by low sperm count, decreased sperm motility and low percentage of normal sperm morphology together or in different combinations. Although many men with varicocele can father children, varicocele causes a progressive time-dependent decline in semen quality. In general, varicoceles do not spontaneously regress. Varicocelectomy is the most common surgical procedure for infertility in males. These include incisional ligation of the veins through the retroperitoneal, inguinal, or subinguinal approaches; percutaneous embolization; and laparoscopy. The goal of treatment of the varicocele is to obstruct the refluxing venous drainage to the testis. The potential complications of varicocelectomy of primary concern are hydrocele formation, varicocele recurrence (failure to decompress the varicocele), and testicular infarction (atrophy).
Materials And Methods
Over a period of 36 months, 76 patients (age 9 to 36 years) underwent LVL for left-sided grade II and grade III varicoceles. Thirty-six patients underwent artery sparing ligation while the other 41 underwent mass ligation. All bilateral varicocelectomies and secondary laparoscopic procedures done for recurrent varicoceles after any other procedure in the form of embolization or high retroperitoneal ligation were excluded from the study.
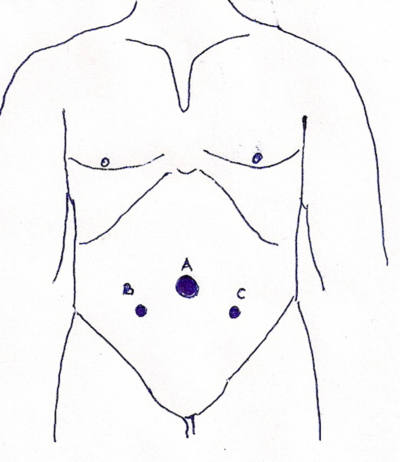
After induction of general anaesthesia, an incision was made just below the umbilicus and a Veres needle was placed into the peritoneal cavity. Four to five liters of carbon dioxide were insufflated through the Veres needle to create a pneumoperitoneum with a pressure of 12 mm Hg. The needle was removed and a 10mm trocar was inserted through the same incision into the peritoneal cavity. A 10mm laparoscope was inserted through the trocar attached to a videocamera and the peritoneal cavity was viewed on a television monitor. In addition to the laparoscope insertion site, at least 2 additional working ports are required to provide access for operating instruments (Fig. 1). One access port is positioned halfway between umbilicus and the ipsilateral anterior iliac spine, and another one is placed in the mirror position on the other side. The internal inguinal ring was identified by the appearance of the vas deferens as it separated from the spermatic cord and entered into the deep pelvis (Fig. 2). The retroperitoneum was incised along the internal spermatic vessels for approximately 1cm using scissors. After the internal spermatic vessels were separated from the underlying psoas major with forceps, they were clamped with clips (Endo Clip II, United States Surgical Corporation, USA). Five to six clips were applied to clamp the vessels. In case of artery preserving ligation, the pulsatile artery was isolated which is easily identified under laparoscopic magnification and the all the rest of the vessels was clipped.
Figure 1
Results
The operative details are shown in Table 1. The average operation time was 36 minutes for LVL with ligation of veins alone and 19 minutes for LVL with mass ligation. There were no preoperative complications in the study group. Among the postoperative complications, hydrocele formation was seen in 4 patients and in 2 patients of the artery-preserved and the artery-ligated group, respectively. Similarly, recurrence was seen in one patient and in no patient, respectively. The average hospital stay was 26 hours and 21 hours, respectively. No patient required opiate analgesia and all returned to normal activity within a few days. At an average follow-up of 24 months (range, 6 to 30) all patients of the artery-preserved and artery-ligated group were asymptomatic and had marked reduction in the size of the varicocele. So far, testicular growth appears to be unaffected and no patient has developed an atrophic testis as a result of the laparoscopic procedure.
Discussion
Traditional surgical correction of varicoceles has been done by ligation of the testicular veins via an inguinal (low/Ivanissevich) or retroperitoneal (high/Palomo) approach. However, these techniques in adolescents are associated with failure rates of approximately 3% to 37%1-3. Embolization of the testicular vein in experienced hands is reported to give better results, but recurrence still occurs in approximately 5%-50%4,5. Also there is a 10 to 20% rate of unsuccessful intervention in the radiologic embolization approach. Venography has shown that the majority of missed vessels lie proximal to the site of vein ligation. In addition, the frequency of missed vessels is higher with a low approach. An approach that enables intraabdominal visualization of the testicular vessels might therefore be expected to reduce the rate of persistent or recurrent varicoceles. Limited data on laparoscopic management of varicoceles in adults give cure rates of 100%. These surprisingly good results may reflect the excellent visibility of the posterior abdominal wall achieved using the laparoscope, which allows a thorough search of sites known to be responsible for recurrent varicoceles, namely renal, vas associated, pelvic, and retropubic cross-over veins. However, in patients who have recurrent varicoceles, the cause appears to be the presence of cremasteric or contralateral scrotal cross-over vessels, which conventional high and laparoscopic approaches may fail to control.
Hydrocele formation is related to failure to preserve the lymphatic vessels associated with the spermatic cord. Franco6 suggests complication rates are relatively low for LVL except for the hydrocele rate, which has been similar to that encountered with the open Palomo approach in case of adolescent male. Keys et al.7 had a hydrocele rate of 12.5%, Pini Prato et al.8 12%, and Méndez-Gallart et al.9 13.5% using laparoscopic mass ligation varicocelectomy. Our study had hydrocele formation in 4 patients (11.42%) when only ligation of veins was done and in 2 patients (4.88%) when mass ligation was done.
Beck et al.10 suggested that unligated small internal spermatic veins may be a cause of varicocele recurrence. Rothman et al.11 also concluded that recurrences are due to either recollateralization or failure to ligate all branches of the venous plexus. Keys et al.7 had a recurrence rate of 8.3% at their center doing laparoscopic mass ligation. McManus et al.12 had none. Méndez-Gallart et al.9 showed that recurrence rates and complication rate of LV are similar to those reported with open surgery. Cimador et al.13 demonstrated that ligation of the artery does not impair testicular growth and thus it is more useful and safe to interrupt the artery to avoid recurrence due to periarterial venous network. Agnifilli et al.14 suggest that laparoscopic high mass ligation of both testicular artery and vein has very low recurrence rates. Similarly, our study had the only recurrence (2.85%) when artery-preserving ligation was done. Kattan et al.15 concluded that LVL with internal spermatic artery ligation has lower recurrence rate than without internal spermatic artery ligation with no increase in hydrocele or testicular atrophy rate. In their study of LVL, Agnifili et al.14 had no signs of testicular atrophy. Our study also had no testicular atrophy. Agnifili et al.14, Pini Prato et al.8 in their nine years of unicentric experience, Méndez-Gallart et al.9 and Keys et al.7, all of them concluded that laparoscopic mass ligation is a highly effective and reliable method for treatment of varicocele. Polok et al.16 also concluded that varicocelectomy using clips gives much less complications than electrocoagulation and should be chosen first. We have also advocated the principle of applying clips throughout. Tong et al.17 demonstated that lymphatic-sparing LVL is a safe, effective and reliable treatment. Huk et al.18 and Parott et al.19 carried on comparative assessment of artery-ligating and artery-preserving varicocelectomy and found that ligation of vein and artery produced better improvement of semen characteristics and percentage of pregnancies in comparison with artery-sparing technique. Even Student et al.20 confirmed using colour Doppler sonography, that ligation of the testicular artery does not lead to major changes in testicular blood supply or sperm quality. Yamamoto et al.21 demonstrated the effect of varicocelectomy on post-operative spermatogenesis and showed that sperm density and motility improved significantly in the artery-ligated group. Yamamoto et al.21, Matsuda et al.22 and Fielder et al.23, all of them concluded that in spite of the advocative advantage of artery preservation, there was no significant difference between artery-ligating and artery-preserving groups when improvements in semen quality and pregnancy rates were assessed. Diamond et al.24 concluded that laparoscopic and Palomo approaches were the most successful. The subinguinal approach (usually incorporating microsurgery and artery sparing) had intermediate success rate and the Ivanissevich approach was least successful.
In our study with Z-test for proportions, to test the significant difference between the two surgical methods, that is venous ligation alone and vein and artery (mass) ligation, a significant difference was observed only for peroperative time, hydrocele and hospital stay at 1% level of significance that is P < .01 (table 1). However, no significant difference was observed for all other parameters between the two surgical methods (P > .01).
Conclusion
LVL is safe, effective, and not very costly, with minimal morbidity, short learning curve and with excellent post-operative results in terms of semen quality and pregnancy rates as compared to the other techniques advocated in the treatment of varicoceles. LVL should preferably be done with en-bloc mass ligation, that is both artery and vein should be ligated. An attempt should be made to spare lymphatics. This requires more training and results in very few hydrocele formation rates. Clips should be used in place of electrocoagulation for mass ligation.