Role of diagnostic laparoscopy in management of acute abdomen
S Mehta, I Juneja, D Udani
Keywords
acute abdomen, diagnostic laparoscopy
Citation
S Mehta, I Juneja, D Udani. Role of diagnostic laparoscopy in management of acute abdomen. The Internet Journal of Surgery. 2008 Volume 20 Number 1.
Abstract
Introduction
Acute abdomen is not a disease itself but a description of a complex of symptoms combined with severe abdominal pain developed within a time frame of less than 24 hours1. All strategies for the management of acute abdomen underline the need for an interdisciplinary approach to diagnosis and therapy. This requires focused and intelligent use of efficient diagnostic procedures. Diagnostic laparoscopy (DL) may be a key to solving the diagnostic dilemma of nonspecific acute abdomen. Furthermore, it allows not only direct inspection of the abdominal cavity but also surgical intervention, if needed2
Diagnostic laparoscopy is a minimally invasive surgical procedure that allows the visual examination of intra-abdominal organs in order to detect pathology.
Diagnostic laparoscopy was first introduced in 1901, when the German surgeon Georg Kelling performed a peritoneoscopy in a dog, which was called “celioscopy”. A Swedish internist named H. C. Jacobaeus is credited with performing the first diagnostic laparoscopy in humans in 1910.3
The diagnostic value of emergency laparoscopy has been proved since the 1950s and 1960s but emergency diagnostic laparoscopy with surgical intervention is recent. It was first proposed by Philippe Moment in 1990.4
Despite new x-ray techniques, or scans, and ultrasound, the diagnosis of acute abdomen can be difficult at times. So far, the most accurate non-invasive method of diagnosis is ultrasound but that is not reliable. History and physical examination will generally lead to correct diagnosis occasionally but diagnostic laparoscopy is the most accurate method even compared to open laparotomy.5
The procedure allows rapid and thorough inspection of the paracolic gutters and pelvic cavity that is not possible with the open approach. The emergency laparoscopic approach for patients with acute abdomen improves the diagnostic accuracy and is therefore nowadays recommended and accepted world wide.6
Aims Of Study
The aims of study are:
1. To evaluate laparoscopy as a diagnostic tool in cases of acute abdomen where other clinical symptoms and investigations are not conclusive.
2. To evaluate benefits and complications of diagnostic laparoscopy.
3. To evaluate the effect of diagnostic laparoscopy on further management of patients with acute abdomen.
4. To know the exact pathology.
5. To avoid unnecessary laparotomy.
Indications
Peritonitis
Mesenteric ischemia
Intra-abdominal abscess not amenable to image-guided drainage
Acalculous cholecystitis
Small-bowel obstruction
Gastrointestinal haemorrhage of unexplained etiology
Appendicitis
Diverticulitis
Gastrointestinal perforation peptic/enteric perforation
Intestinal adhesion
Bedside laparoscopy in ICU
Torsion of intra-abdominal testis
Contraindications
1. An active infection of the anterior abdominal wall near the planned entry or accessory trocar site is an absolute contraindication to performing diagnostic laparoscopy.
2. Lack of cooperation is a contraindication when utilizing local anesthesia.
3. Uncorrectable coagulopathy is a contraindication, but minor degrees of coagulopathy are no contraindication to diagnostic laparoscopy.
4. Obesity and previous surgery are no contraindication to diagnostic laparoscopy.
When performing under general anaesthesia, patients with cardiac diseases, COPD, diminished cardio-pulmonary reserve or previous extensive abdominal surgery are no good candidates for diagnostic laparoscopy.
Advantages
Cosmetically better outcome, small incision, so smaller scar.
Smaller incision leads to less damage and less tissue stretching leading to less postoperative pain.
Retraction is provided by low-pressure pneumoperitoneum giving a diffuse force applied gently and evenly over the whole abdominal wall causing minimal trauma and less damage of serosal covering. So there are less chances of postoperative adhesions.
Better visualization of paracolic gutters and pelvic cavity which is not possible by diagnostic laparotomy.
Disadvantages
As compared to USG, CT and MRI, diagnostic laparoscopy is an invasive procedure, so there are more chances of complications.
For diagnostic laparoscopy, also special costly instruments and special training are required.
Instruments of diagnostic laparoscopy are longer and more complex to use than in open surgery and a significant hand-eye co-ordination problem may occur in trainees.
In case of intra-operative arterial bleeding, hemostasis is difficult to achieve and so conversion to open surgery may be needed.
Complications
Laparoscopy is associated with unique risks and complications that do not exist with open surgery. The most important of these complications are major vascular injuries, intestinal injuries, and CO2 embolism, any one of which is potentially lethal.
The mortality from several large series of diagnostic laparoscopy has averaged 0.05% with a range of 0.014% to 0.13%. Major complications have occurred in 0.15% to 0.6% of cases with an average rate of 0.38%.
Intestinal and vascular injuries occurred in 0.14% and 0.25% of cases, respectively. Complications that required laparotomy occurred in 1.2% of patients.
Trocar injuries may occur with either a closed or open insertion technique, although the risk is greater with the closed method, especially during blind insertion of the first trocar. Excessive use of force is often a factor in such injuries.
Most insertion-related vascular complications involve the aorta, inferior vena cava, iliac artery and vein, or mesenteric vessels. Injuries incurred with the Veress needle sometimes can be managed conservatively if the patient is stable and the site of injury is inspected carefully after laparoscopic access to the peritoneal cavity has been gained. Trocar injuries to major intra-abdominal vessels always must be treated by open laparotomy. Exclusion of such injuries should be the first priority of the laparoscopist following insertion of the initial trocar and video telescope. Major vascular injury always should be suspected in any patient who experiences sudden hemodynamic collapse during a laparoscopic procedure.
In such cases, one should discontinue gas insufflation immediately and quickly lower CO2 pressure to 8mmHg, because of the possibility of a CO2 embolism. The endoscope should not be removed, but a rapid scan of the abdomen and retroperitoneum should be carried out with the video telescope to search for hemorrhage. If retroperitoneal blood or retroperitoneal hematoma is present, an exploratory laparotomy should be performed immediately and the bleeding site compressed until the patient has been stabilized. Delay in performing laparotomy on the patient with a major vascular injury only increases the risk of exsanguination and death. Sudden hemodynamic collapse of the patient undergoing laparoscopy may also result from CO2 embolism, tension pneumothorax, or cardiac dysrhythmias.
Injuries to the gastrointestinal tract may be incurred at any point during the laparoscopic surgical procedure. The management of intestinal injuries from laparoscopy depends on the extent of the injury. Suspected injuries due to the Veress needle first should be inspected carefully with a laparoscope after gaining access at an alternative site; treatment may consist of either observation or laparoscopic suturing of the injury. If intestinal laceration occurs with the trocar, the trocar should be left in place while an open laparotomy is performed. Management of trocar injuries to the bowel with laparoscopic techniques may be possible in carefully selected cases. Gastrointestinal injuries also may occur from electrocautery and laser burns or from lacerations by laparoscopic instruments. If unrecognized, such injuries may result in delayed perforation with peritonitis, sepsis, and death.
The risk of bladder injury during trocar insertion should be minimal if the bladder has been decompressed with a Foley catheter. Lacerations to solid organs (liver, spleen) may occur from laparoscopic instruments or when an upper abdominal alternative insertion site is used. Abdominal wall complications that may occur owing to trocar injuries include bleeding, hematomas, and hernias. Injury to abdominal wall vessels (e.g. inferior epigastric artery usually can be avoided by transilluminating the abdominal wall with a laparoscope before placing the trocar. Inspection of all trocar sites at the completion of the laparoscopic procedure should be performed routinely to avoid unrecognized bleeding from these sites. Hernias that develop postoperatively through a laparoscopic port site have a high incidence of incarceration and Richter hernia formation because of the small size of the fascial defect. Closure of the fascia at all port sites 5mm or greater in diameter is recommended to avoid this complication.
A number of complications may develop as a result of CO2 pneumoperitoneum. These include CO2 embolism, hypercarbia, subcutaneous emphysema, and rarely, pneumomediastinum and pneumothorax. Improper placement of the Veress needle also may result in insufflations of the preperitoneal space or CO2 emphysema involving the omentum, intestinal mesentery, and retroperitoneum. Hypercarbia and the accompanying acidosis usually can be managed by increasing minute ventilation and lowering the CO2 insufflation pressure. Subcutaneous emphysema may exacerbate the degree of hypercarbia, but it is otherwise of no consequence clinically and usually resolves within 24 to 48 hours of surgery. Cardiac complications of pneumoperitoneum include transient dysrhythmias and bradycardia from increased vagal stimulation.
Material & Method
Laparo = Abdomen, scopy = to visualize
Laparoscopy is defined as endoscopic visualization of the interior of the abdominal cavity.
Equipments:
The equipments and instruments used for diagnostic laparoscopy are as below:
The video camera is attached directly to the laparoscope and contains both a manual focus mechanism and a zoom capability. The essential electronic component of the video camera is a solid state chip sensor or a charged coupled device (CCD). The CCD functions as an electronic retina that transmits light received from the laparoscope into an electronic signal and then is transduced into a video image. The CCD itself comprises numerous light-sensitive photodiodes, or pixels. Light activation of an individual pixel results in the generation of an electronic signal that is conducted via cable to the camera control unit. The camera control unit then processes this signal and reconstructs the image on the video monitor using conventional horizontal scanning.
The quality of the video image depends on several technical factors, including resolution, color, light sensitivity, signal to noise ratio and image size. The degree of resolution of the video cameras is determined by the number of pixels in the CCD. The minimal resolving power required for the video camera for operative laparoscopy should be 400 lines of resolution per inch. Most laparoscopic cameras currently in use have a single chip sensor that provides a resolution of 450 horizontal lines per inch. Newer three-chip cameras also have been developed that provide up to 700 lines per inch and improve chromatic accuracy.
High-resolution video monitors are required for suitable reproduction of the endoscopic image. In general, the resolution capability of the monitor should match that of the video camera such that a one-chip camera is best coupled with a monitor that provides at least 400 lines per inch. Three-chip cameras require more expensive monitors with 700 lines per inch to realize the improved resolution of the extra chip sensors.
One or if possible two separate video monitors, placed on the side of the operating table, are commonly used for most laparoscopic cases, allowing all members of the surgical team an unobstructed view of the operation. Additional monitors may be useful for some advanced laparoscopic procedures. The screen size of the video monitor ranges from 13 to 21 inches. Resolution capacity of video monitor is 640 x 480 lines per inch.
A neon light source is required for adequate visualization of the operative field. It approximates bright sunlight and is ideal for visual and photographic colors.
It pumps CO2 from a cylinder of pressurized gas through a regulator and into the abdomen at a set rate and pressure. The CO2 is delivered at a predetermined flow rate and has a pressure setting that, if exceeded, shuts off the flow of gas. It should be able to deliver at least 6L of gas per min.
This is a device to irrigate and aspirate blood, bile, debris and fluid for diagnosis.
These devices are used for hemostasis. Care must be taken in using the cautery to prevent spark gap injury to bowel or other organs. A laser uses photons as its energy source to cut and coagulate tissue.
Instruments:
Most of the instruments have a design similar to those which are in use in general surgery.
Insertion of a needle into the peritoneal cavity is necessary to establish the pneumoperitoneum. The standard length is 10 cm.
Magnification is up to 20 times. Endoscopes come in multiple sizes with 10mm, 5mm, and also 2mm and 3mm. They are either end-viewing (viewing the field directly in front of the lens) or angled (viewing an oblique area from the end of the lens). The most commonly used angled scope is 300.
The most common cannula sizes are 11 mm, 10mm and 5.5 mm. The trocar has a pyramidal tip and needs to be sharpened periodically.
The jaws can be single-action (one jaw is fixed and the other one moves) or double-action (both jaws move).
The safest one is with a blunt tip. The Maryland or Zucker dissector is effective with cystic structures.
The most common coagulating instruments are the hook and the spatula.
Scissors are used to break adhesions.
They are tubes that are placed in 10mm or 11mm reusable cannulas to reduce the diameter of the Trocar for smaller instruments.
They reduce the opening at the top of a disposable cannula from 11mm to 10.5mm and from 11mm and 10mm to 4.5mm and 3.5 mm.
Procedure:
Diagnostic laparoscopy in the patients presenting with acute abdominal pain is performed as below:
PATIENT POSITION:
The patient is placed on the operating table with the legs straight.
The patient must be positioned properly at the beginning of the procedure, making certain that all pressure points are padded.
The operating table is tilted head up or down by approximately 15 degree depending on the main area of examination.
Compression bandage may be used on legs during the operation to prevent thromboembolism.
The surgeon stands on the left side of the patient.
The first assistant, whose main task is to position the video camera, is also on the patient’s left side.
The instrument trolley is placed on the patients left allowing the scrub nurse to assist the placing of appropriate instruments in the operating ports.
Television monitors are positioned on either side of the top end of the operating table at a suitable height; so surgeon, anesthetist, as well as assistant can see the procedure.
ANAESTHESIA:
Local anaesthesia can be injected into the skin of the abdominal wall to completely numb the area and allow safe placement of the laparoscope. A small dose of IV sedation is also given.
General anaesthesia is of choice, as we can even do therapeutic management after doing diagnosis.
Prophylactic antibiotics are generally not indicated in diagnostic laparoscopy but in tropical countries like India it is advisable to use prophylactic antibiotics.
CREATION OF PNEUMOPERITONEUM:
The subcutaneous tissue is bluntly dissected until the umbilical fascia is palpable. The abdominal wall inferior to the umbilicus then is lifted with one hand while the Veress needle is inserted through the fascia at the base of the umbilicus at 450 toward the pelvis so as to prevent injury to aorta and IVC. Two clicks of the Veress needle will be appreciated as it penetrates first the fascia and then peritoneum. Intraperitoneal placement is confirmed by free movement of the needle.
Saline drop test: The needle is filled with saline and fluid is sucked into the peritoneal cavity by the negative pressure created inside.
Aspiration with no return of blood or bowel contents.
Irrigation with free flow of fluid.
Zero or negative pressure on CO2 insufflator display.
The needle is now attached to the insufflator which delivers the CO2 at a rate of 1l/min. initially. The pressure is maintained at 10-12mm of Hg; 2-3l of gas is usually required for an average adult to establish pneumoperitoneum upon which the abdomen distends symmetrically and becomes tympanic and liver dullness obliterated. The needle is removed and replaced by a 10mm trocar and cannula grasped in the palm of one hand and inserted using gentle, firm pressure while elevation the abdominal wall with the other hand and aiming at the sacral hollow. Once inside, the trocar is removed, the cannula is advanced for a short distance and the telescope is inserted, to which insufflator and light source are attached.
The fascia and peritoneum are incised under direct vision. Once the peritoneum is opened, the placement of the Hasson cannula requires taking the simple sutures in either side of the fascia. The cannula tip is inserted through the opening and the sutures are pulled up tightly around the wings of the cannula.
In small children and infants the umbilicus must be avoided because accompanying umbilical abnormalities may be expected in a large percentage of cases. Veress needle and first trocar are placed in the suprapubic area lateral to the rectus muscle on the left side. This point is called “point of Munro”.
Then, according to requirement, accessory ports are placed.
The open technique for trochar insertion is recommended if a patient presents with severe abdominal distention. Nitrous oxide is used if diagnostic laparoscopy is performed in local anaesthesia because nitrous oxide has its own analgesic effect. Carbon dioxide is the preferred gas if the procedure is performed under general anaesthesia. Insufflation should be very slow and with care taken not to exceed 12mm of Hg.
PORT LOCATION:
Generally, one optical port at the umbilicus and one 5mm port in the left iliac fossa are required.
A three-port approach should be used if there is any difficulty in manipulation.
10mm: umbilical (optical)
5mm: suprapubic
5mm: right hypochondrium
A 30-degree telescope is employed in most instances, as this facilitates easier inspection of peritoneal cavity and abdominal organs. The secondary ports are inserted under laparoscopic vision. The selected site on the abdominal wall is identified by finger identification of parietal peritoneum.
The usual site of insertion of the trochar cannula for diagnostic laparoscopy is below or to the side of the umbilicus. This position may require to be altered in the presence of abdominal scars. The use of a 30-degree forward oblique telescope is preferable for viewing the surface architecture of organs. By rotation of the telescope, different angles of inspection can be achieved.
The first important step after access to the abdomen has been gained is to check for damage caused by trochar insertion A second 5mm port may then be inserted under vision in an appropriate quadrant to take a palpating rod.
Patient in steep Trendelenburg position.
Reverse the Trendelenburg tilt.
INSPECTION OF PELVIS
Patient should again be positioned in steep Trendelenburg position.
The full length of the fallopian tube
Round ligament
Anterior cul de sac
Uterus
A systemic examination of the abdomen must then be performed as in laparotomy. We begin at the left lobe of the liver but any scheme can be used as long as it is consistent. Next, check around the falciform ligament to the right lobe of liver, gallbladder and hiatus. After checking the stomach, move on the caecum and appendix and check the terminal ileum, follow the colon round the sigmoid colon, and then check the pelvis. You should be conversant with use of position and manipulation to aid vision. This is the first procedure to be mastered when learning laparoscopic surgery.
During diagnostic laparoscopy:
The abdominal cavity is inspected for fluids.
A sample is taken if free fluid is present for laboratory tests (chemistry, bacteriology).
Peritoneal lavage and adhesiolysis may need to be performed to improve visualization of organs.
Impact of diagnostic laparoscopy on management:
(1) If no pathology is to be treated with surgical intervention, then complete the diagnostic laparoscopy, remove instrument and gas and close the port site.
(2) If a pathologic finding needs surgical intervention (e.g. acute appendicitis) then do it laparoscopically (laparoscopic appendicectomy).
(3) If laparoscopic management is not possible due to any reason, convert to laparotomy.
Below are some of the pictures caught during diagnostic laparoscopy.
Observation And Results
In this prospective study to evaluate usefulness of diagnostic laparoscopy as diagnostic tool we found the following observations.
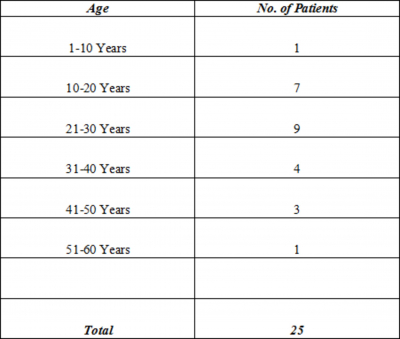
Here we have studied the patients with age range from 10 yrs to 55 yrs. Pediatric and elderly patients were not included in the study.
In our study, there were 72% male patients compared to 28% females.
Here, in two patients, there was some definitive pathology on clinical grounds not detected on DL and one patient had a normal study.
Among 25 patients, sixteen were treated laproscopically, five with the open method and no surgical intervention was done in four patients.
Discussion
This study, “Diagnostic laproscopic in management of acute abdomen” was performed in Guru Gobind Singh Hospital, Jamnagar, on patients admitted with the complaint of acute abdominal pain in the Trauma Ward in the years 2006-2007.
Here, we had randomly selected patients with acute abdomen, diagnostic laproscopy was performed and on the basis of DL results, we proceeded to surgical intervention.
We included patients from all age groups starting from 10 yrs to 55 yrs. Patients below the age of 10 yrs and above 55 yrs were excluded. Our study included 72% male and 28% female patients. Male preponderance is due to specific disease epidemiology and also to gynecological pathology that we have not included in our study. We have not studied those patients who present with acute abdominal conditions in the gynecological department.
Out of all patients submitted to diagnostic laparoscopy, 8 patients (32%) presented with acute appendicitis, 5 patients (20%) with peptic perforation, 2 patients (8%) with enteric perforation, 2 patients (8%) with Koch's abdomen, one each with acute pancreatitis, obstruction, Meckel's diverticulitis, ectopic testis, and primary peritonitis.
Without doing diagnostic laparoscopy, we reached diagnosis on the basis of clinical findings, physical examination, x-rays and ultrasound of the abdomen and on that diagnosis, we proceeded to further management that may be operative intervention in the form of exploratory laparotomy or we treated the patient conservatively in absence of diagnostic proof. In cases which were treated conservatively and later on underwent exploratory laparotomy, there was increased morbidity, hospital stay, and treatment cost both to government and patient, with loss of many man hours.
In all 25 patients of our study, we performed diagnostic laparoscopy with the help of one 10mm optical port at the umbilicus and one 5mm port at the left iliac fossa and we reached a final diagnosis which was just confirmation of diagnosis by conventional methods in 16 patients (64%), but in 6 patients (24%) diagnosis was changed.
Excluding those patients who had a pre-DL diagnosis of acute appendicitis, which was confirmed after DL, the remaining 17 patients were supposed to undergo exploratory laparotomy, but with the help of DL we reached a correct diagnosis and prevented unnecessary exploratory laparotomy in 13 patients. Only four patients underwent laparotomy. So,
Whenever there is no availability of laparoscopy, we used to perform exploratory laparotomy with long, usually midline vertical incision extending above and below the umbilicus, but if we do diagnostic laparoscopy first we do not need to perform exploratory laparotomy as we manage the problem laparoscopically. Even if we need to do laparotomy, it will be a small incision as we know the exact pathology. Our data says that we have done only 4 laparotomies:
2 paramedian incisions: Both ileal perforations
4 laparotomies:
Trichobezoar
2 midline incisions:
Sealed peptic perforation
Both ileal perforations were closed with small paramedian incisions and two patients, one with trichobezoar and one with sealed peptic perforation were operated with small midline incisions; thus,
Only one patient out of 16 managed laparoscopically developed a post-operative complication, a pelvic collection which was of very minimal amount and resolved by antibiotics; but 2 patients out of five managed by open surgical procedure developed complications like paralytic ileus and wound infection. But no one had major post-operative complications that needed major intervention. By reducing operative time, exposure to environment and incision length,
Conversion Rate:
Out of 21 patients, in whom we tried to operate laparoscopically, 4 went to laparotomy, 2 because of difficult procedure and 2 because of failed diagnosis. So, in our study,
In this study, 25 patients were exposed to diagnostic laparoscopy. Among them, in two patients diagnostic laparoscopy did not reach the correct diagnosis and failed. One was having a terminal ileum trichobezoar which is an intraluminal pathology and as laparoscopy lacks tactile perception, we failed to diagnose the pathology and another patient was having severe abdominal pain with free gas under the diaphragm with fever; we did not reach the definitive diagnosis and on laparotomy we found a sealed-off perforation on the lesser curvature of the stomach.
We analyzed the histopathological reports of all specimens send for examination. All histopathology reports were supporting the diagnosis made by diagnostic laparoscopy except one case in which DL was suggestive of primary peritonitis but on USG there were worms in the small intestine, so the surgeon had done prophylactic appendectomy and sent the specimen for histopathology report which was suggestive of chronic appendicitis with adult worms in the lumen.
Conclusion
After using diagnostic laparoscopy in management of acute abdomen, we came to the conclusion that diagnostic laparoscopy is helpful in diagnosis. It reduces the chances of unnecessary laparotomy. By exact diagnosis, diagnostic laparoscopy reduces scar size, complications related to surgery, operative time and hospital stay and thus it reduces morbidity and mortality. Diagnostic laparoscopy is the gold standard15 in management of acute abdomen as it is easy, less time consuming, cosmetic and definitive with lesser complications and lesser morbidity and mortality.
By appropriate training, enough experience, enough patience and proper selection of the patients, the result of diagnostic laparoscopy is best and it is the best diagnostic test available at present.