Esophageal atresia with distal tracheoesophageal fistula with gasless abdomen: a diagnostic dilemma
Z Hasan, V Upadhyaya, P Srivastava, S Sharma, A Gangopadhyay
Citation
Z Hasan, V Upadhyaya, P Srivastava, S Sharma, A Gangopadhyay. Esophageal atresia with distal tracheoesophageal fistula with gasless abdomen: a diagnostic dilemma. The Internet Journal of Pediatrics and Neonatology. 2008 Volume 9 Number 2.
Abstract
A “gasless abdomen” in babies with esophageal atresia (EA) has traditionally been thought to imply absence of a distal tracheoesophageal fistula (TEF). We present 2 cases with gasless abdomen and later turned out to be cases of esophageal atresia with tracheoesophageal fistula. These cases are presented because of its extreme rarity and because of ease in management if the condition is diagnosed preoperatively.
Introduction
A gasless abdomen in a neonate with esophageal atresia (EA) implies the absence of a distal tracheoesophageal fistula (TEF) and that the lesion is either an isolated atresia or associated with a proximal fistula. These children usually have a gastrostomy as their initial management and this may create respiratory problem in such patients because of low pressure zone through gastrostomy tube as happened in one of our patient. Goh. D W et al [1] reported 5 such cases and suggested that this variant of tracheoesophageal fistula can be expected in at least 14% of patients presenting with a gasless abdomen, but even on extensive search we found only three more reported cases. These cases are presented because of their rarity and difficulty in management of such patients if not diagnosed prior to surgery.
Case 1
A fullterm male baby presented with copious salivation through mouth and respiratory distress after 48 hr of birth. On examination respiratory rate was 58/min, peripheral cyanosis was present and abdomen was not distended. We were not able pass red rubber tube beyond 10 cm from the upper incisor. X-ray baby gram showed red rubber tube coiled in the esophagus and there was no gas in the abdomen. The patient was adequately resuscitated and treated with feeding gastrostomy and cervical esophagostomy. After operation the patient developed respiratory distress and became cyanosed and on examination gush of air was heard coming through the gastrostomy tube because air bypassed the lung and got to the stomach due to opening of blocked fistula. A diagnosis of esophageal atresia with distal tracheoesophageal fistula was made and patient underwent thoracotomy and fistula ligation. The patient did well in post operative period and later reverse gastric tube esophageal replacement was done.
Case 2
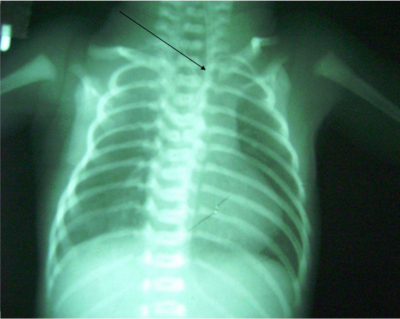
A full term low birth weight baby presented with excessive salivation form mouth after 72 hrs of birth and an X- ray (done after 48 hrs of birth) revealed gasless abdomen (figure – 1)
Figure 1
On examination respiratory rate was 64/min, cyanosis and signs of pneumonitis were present, feeding tube could not negotiated into the stomach. Diagnosis of pure esophageal atresia was made. Patient was resuscitated with nebulization, endotracheal suction and bag and mask ventilation.
Repeat X-ray (figure – 2) done after 48 hours to assess the lungs , showed small amount of gas in the intestine and pneumonitis which was suggestive of esophageal atresia with distal tracheoesophageal fistula. Patient underwent primary extrapleural repair and did well in the postoperative period.
Discussion
Esophageal atresia is a relatively common congenital anomaly with an incidence of 1 in 2500 to 3000 live births [2]. The original classification of this condition was by Vogt in 1929, and this was later modified with the addition of numerous subtypes by Kluth in 1976 [3]. EA with distal TEF is the most common variety and is distinguished by the presence of air in the stomach. It has been noted, however, that up to 1.5% of cases with this anomaly will have a gasless abdomen owing to an atretic segment of the fistula, a mucous plug blocking the fistula, or a membrane in the distal esophagus [2] [4] and [5]. It is important to pick up this small subset of patients because they are amenable to early repair. Goh et al [2] recommended that all children with TEF and a “gasless abdomen” should have a bronchoscopy to look for a distal fistula and to diagnose associated proximal fistulas. They also recommended preoperative contrast studies and passage of sounds via a gastrostomy to assess the distal esophagus. Using these methods, they found 14% of patients with a gasless abdomen in their series had a distal TEF but we observed only two such cases. C.K. Sinha et al [6] reported a variant of gasless abdomen in a case where the TEF was between the lower pouch and the trachea, with a cystic dilatation in the mid portion. The tracheal end of the fistula was obstructed by a membranous septum at both ends of a cystic dilatation; leading to a diagnosis of pure EA. Ozacn C et al [7] reported a case of esophageal atresia with obliterated distal tracheoesophageal fistula because of presence of heterotrophic pancreatic tissue. Wolfgang Lambrecht et al [8] reported a case of esophageal atresia with distal tracheoesophageal fistula with gasless abdomen where the fistula was obliterated due to presence of additional membrane in distal esophagus. One would assume that with the presence of a patent fistula, air would appear in the stomach even with the first breath. The cases in our study have shown that the absence of gas in the stomach on x-ray does not necessarily mean the absence of a distal fistula, because some time fistula is very narrow and may be blocked by mucous plug which may become patent later on while resuscitating the patients. It seems that nebulization and proper resuscitation lead to the dislodgement of mucous plug in one of our case. We suggest that a repeat x ray chest should be done in all cases of pure esophageal atresia after proper resuscitation to rule out patent distal tracheoesophageal fistula because it will avoid unnecessary laparatomy in these patients.
Correspondence to
Dr. Zaheer Hasan Department of Pediatric Surgery IMS, BHU, Varanasi India drzaheerhasan@yahoo.com