Isolated Left Upper Lobe Aplasia And Lower Lobe Hypoplasia With Bronchial Asthma
R Kushwaha, S Verma, V Mahajan, R Singh, R Prasad
Keywords
aplasia, bronchial asthma, hypoplasia
Citation
R Kushwaha, S Verma, V Mahajan, R Singh, R Prasad. Isolated Left Upper Lobe Aplasia And Lower Lobe Hypoplasia With Bronchial Asthma. The Internet Journal of Pulmonary Medicine. 2006 Volume 9 Number 1.
Abstract
Congenital malformations like hypoplasia or aplasia of the lung with bronchial asthma are rare clinical conditions. Here we are reporting such type of case in a 36 years old non smoker male.
Introduction
Pulmonary hypoplasia or aplasia is a rare condition and characterized by incomplete development of lung tissue as a result of embryological defects. It is usually unilateral and is associated with congenital defects which involve skeletal, cardiovascular, gastrointestinal and genitourinary system1. The exact etiology of this condition is not known. It usually presents in childhood but may present later in life. Association of bronchial asthma with pulmonary hypoplasia or aplasia is very uncommon2 which prompts us to report this case.
Case Report
A 36 year old non smoker man was admitted to our department with complaints of cough with expectoration and episodic breathlessness since early childhood. Previously he had received two adequate courses of primary line anti tuberculosis drugs without any clinico-radiological improvement. His resting pulse rate was 92 / min, blood pressure was 128/74 mmHg and respiratory rate was 24 / min. Respiratory system examination revealed flattened left side chest with ipsilateral mediastinal shift and also there were reduced chest movements on the left side. Percussion note was dull on the left side. Breath sounds were normal vesicular in character on the right side with random polyphonic rhonchi but the intensity of breath sounds on the left side was grossly reduced. Heart sounds were normal. Chest x-ray showed complete opacification of left hemithorax with hyperinflation of right lung and herniation with sifting of mediastinum to left lung (Fig: 1).
Figure 1
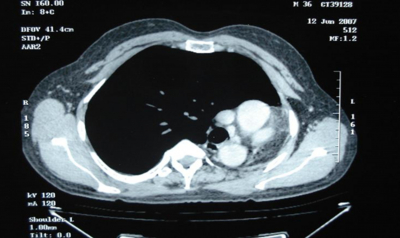
Sputum for AFB smear on three consecutive days was negative. His Haemoglobin was 12 gram %; total leucocyte count 8100/cmm: neutrophils 72 %, lymphocytes 25 % and eosinophils 3%. His blood urea was 28 mg/dl; serum creatinine 0.5 mg/dl. His serum bilirubin was 0.6 mg/dl; SGPT 28 U/L; SGOT 19 U/L, SAP 193 U/L. Spirometry showed forced expiratory volume in one second (FEV1%) of 48 and FEV1of 770ml (24% of predicted). There was a significant reversibility of 230 ml in FEV1 after inhaled salbutamol. Thus diagnosis of bronchial asthma was made. Subsequently his CT was done that revealed small left main bronchus with very small left lower lobe bronchus (Fig: 2).
Figure 2
Left upper and lingular lobe bronchi were absent with no lung tissue of upper and lingular lobes of the left lung. The right lung was overinflated with compensatory emphysematous changes. On contrast administration, the left pulmonary artery was normal in caliber; however, branching to upper and lingular lobes was not seen. His Fiberoptic bronchoscopy revealed a short left main bronchus with absent left upper lobe bronchus. The left lower lobe bronchus was very narrow and the scope could not be passed forward. On the right side the tracheobronchial tree was normal. His MRI thoracic angiography was done that did not reveal any vascular anomaly (Fig: 3).
His USG abdomen was normal. Thus diagnosis of left upper lobe aplasia with left lower lobe hypoplasia with bronchial asthma was made. The patient's symptoms breathlessness relieved were abolished after initiation of inhaled bronchodilator and corticosteroids with oral mast cell stabilizer.
Discussion
Agenesis of the lung is an extremely rare congenital anomaly representing failure of development of the primitive lung bud. This condition was first described by De Pozze, who discovered it accidently at the autopsy of an adult female in 16733. Munch Meyer first diagnosed unilateral agenesis of the lung clinically in 18854. From India, the first case was reported by Muhamed in 1923, of a left sided pulmonary Agenesis5. Pulmonary agenesis is classified into three categories depending upon the stage of development of the primitive lung bud6: (1) Agenesis—Complete absence of lung and bronchus and no vascular supply to the affected side, (2) Aplasia—Rudimentary bronchus with complete absence of pulmonary parenchyma (Left Upper Lobe aplasia in present case) (3) Hypoplasia—Presence of variable amounts of bronchial tree, pulmonary parenchyma and supporting vasculature (left lower lobe hypoplasia in present case). The causes of pulmonary hypoplasia may be primary (deficient TTF-1, GATA factors, hepatocyte nuclear factor HNF310, epidermal growth factor and its receptor, EGFR; mitogen-activated protein [MAP] kinase, but it is usually secondary (small fetal thoracic volume, prolonged oligohydramnios, early rupture of membranes at 15-28 weeks' gestation7, longer latent period before delivery, decreased fetal breathing, congenital heart diseases and trisomies 18, 13, 21) 8. The true incidence is unknown. No sex predilection has been noted. Congenital lung defcts with bronchial asthma is very rare9. Till now only three cases are reported2,9,10.
The onset of symptoms in pulmonary agenesis is remarkably variable. In many cases, presence of this anomaly usually comes to light during infancy because of recurrent chest infections, cardio-pulmonary insufficiency or due to associated congenital anomalies11. Nearly 50% cases of pulmonary hypoplasia or aplasia have associated congenital defects, which usually involve cardiovascular, skeletal, gastrointestinal and genitor-urinary system7.
Chest radiograph usually reveals homogenous density on the involved side. Other findings are mediastinal shift, compensatory herniation of the contralateral lung across the mediastinum, bell-shaped chest, and rib deformities. CT Thorax is now emerged as diagnostic modality of choice. It helps to delineate pulmonary parenchyma, pulmonary vasculature and the bronchus, while CT angiography and echocardiography detail the pulmonary vasculature. With the advent of these techniques, the exact diagnosis can be established without opting for invasive procedures like bronchography and pulmonary angiography 12,13,14.
In roentgenographic differential diagnosis of hypoplasia or aplasia are collapse, thickened pleura, destroyed lung and pneumonectomy . Surgery is seldom required for agenesis or aplasia, which can be managed on conservative lines. The prognosis of such cases depends upon the functional integrity of the remaining lung as well as upon the presence of associated anomalies.
Our report highlights the fact that a high index of suspicion is required to diagnose congenital lung anomalies, and that asthma can occur in such patients. Appropriate anti-asthma therapy can alleviate symptoms and reduce morbidity.
Correspondence to
Dr. R.A.S.Kushwaha M.D. Assistant Professor Department of Pulmonary Medicine C.S.M. Medical University, Lucknow (India)- 226003 Phone: 0522-2255167 Email: kushwaharas_kgmu@rediffmail.com