Misdiagnosis of COPD in middle-aged asthmatics in Nepal
M Nepal, M Bhattarai
Keywords
asthma, copd, misdiagnosis, reversibility
Citation
M Nepal, M Bhattarai. Misdiagnosis of COPD in middle-aged asthmatics in Nepal. The Internet Journal of Pulmonary Medicine. 2007 Volume 10 Number 1.
Abstract
The study was conducted at the Department of Medicine, Bir Hospital, National Academy of Medical Sciences (NAMS),a national postgraduate hospital and referral center, Post Box: 3245, Kathmandu, Nepal.
FEV1 = Forced Expiratory Volume in one second; FVC = Forced Vital Capacity.
The study was designed to find out the proportions of reversible asthma among 35–69 years old patients with COPD. There are reports suggestive of misdiagnosis of COPD in the elderly asthmatics in the industrialized countries; however studies are limited from developing nations and even rare in young populations. Such study about misdiagnosis of COPD in asthmatics in younger age may warrant further investigations.
Introduction
In adults asthma may manifest during early or late adulthood or even old age. There are reports suggestive of misdiagnosis of COPD in elderly asthmatics in industrialized countries. 1,2,3 In this region, COPD is frequently encountered in middle-aged subjects. Crude prevalence rate of chronic bronchitis and cor-pulmonale have been reported to be 11.3% to 30.9% and 0.5% to 5.6% respectively among people with mean (SD) age 40 (15) years in different parts of Nepal. 4 In a study of cor-pulmonale due to COPD in Nepal, the mean age(
Methods
Subjects
We studied total 60 patients 35 to 69 years-old, with history of chronic cough, dyspnoea and wheezing, who were being treated with a presumed diagnosis of COPD for at least 1 year and were not receiving systemic or inhaled corticosteroids. Patients were included if their X-ray chest and ECG were, apart from showing features consistent with COPD, otherwise normal and if their postbronchodilator spirometry showed airflow limitation (FEV1/FVC < 0.7). Patients with features suggestive of bronchiectasis, cor pulmonale or cardiac diseases had been excluded from the study. Consecutive patients attending the hospital who fulfilled the inclusion and exclusion criteria were included. All patients underwent a thorough history and physical examination, and routine haematocrit and biochemistry, chest radiograph, resting ECG and baseline and repeat spirometry examinations after bronchodilator and oral corticosteroids. The study was approved by Nepal Health Research Council in March 2002. Written informed consent was obtained from all subjects. Arrangements were made to refer the patients later after study to appropriate units to manage them as per their clinical condition and investigation results. The study was conducted in Bir Hospital, the national postgraduate and tertiary referral hospital from April 2002 to March 2003.
Spirometry
Forced Expiratory Volume in one second (FEV1) and Forced Vital Capacity (FVC) were measured by the investigators with a vital graph (Model S; Vital Graph Limited; Maids Moleton House Buckingham MK-18) following the recommended standard techniques and calibration. 6,7 The spirometry test was done by one of the investigators, who had been doing it regularly, with emphasis on maximal patient effort in performing the test. Baseline FEV1 and FVC were recorded until three acceptable and reproducible recordings differing <5% were obtained. Maneuvers were accepted as technically satisfactory if the back extrapolated volume was <0.15 L or 5% FVC, and if the expiratory time was at least 6 s. Highest values were used for analysis. As aim of the study was to see the degree of reversibility of airflow limitation, the spirometry was performed when the patients were clinically stable and free from respiratory infection. For repeat testing also the equipment and operator were the same and the time of the testing was within 2 h of previous test times. Smoking was avoided for more than 1 h prior to testing and throughout the duration of test procedure. Short-acting inhaled drugs like salbutamol or ipratropium were stopped at least 6 h before testing. Long-acting bronchodilators like salmeterol and twice a day preparations of oral theophylline or slow-release beta agonists were stopped for 12 h prior to the test and once a day sustained release preparations for 24 hours.
Reversibility testing
Reversibility testing of airflow limitation was done both after inhaled bronchodilator and oral corticosteroids. 8,9 For bronchodilator reversibility testing, the patients were asked, after a gentle and incomplete expiration, to inhale a dose of 100 microgram of salbutamol in one breath to total lung capacity from a metered dose inhaler with a valved spacer device. The breath was then held for 5-10 s before the patient exhaled. Four separate doses (total dose 400 microgram) were given at around 30-s intervals. Spirometry was repeated after 15-min. For corticosteroids reversibility testing, spirometric values were also measured at the end of two-week course of oral prednisolone 30 mg per day. The criteria for FEV1 response were as for bronchodilators. Using percent change from the baseline as the criterion, both ≥12% and ≥15% increase in FEV1 following bronchodilator or corticosteroids were considered as showing reversibility of airway and included as bronchial asthma. 8,9,10 Thus in the present study, bronchial asthma was diagnosed when all the following criteria were fulfilled: (1) 35 to 69 years-old patients with history of chronic cough, dyspnoea and wheezing for at least 1 year without any features suggestive of bronchiectasis, cor pulmonale or cardiac diseases and with otherwise normal X-ray chest and ECG, (2) postbronchodilator spirometry showing airflow limitation (FEV1/FVC < 0.7), and (3) ≥12% or ≥15% increase in FEV1 following bronchodilator or corticosteroids.
Statistical analysis
Data were analyzed with a statistical software package (SPSS, version 10.0 for Windows; SPSS Inc; Chicago, IL). Mean values with standard error (Mean ± SE) were calculated along with 95% confidence interval (CI) as applicable. The chi square test was used to assess the differences in the percentages of patients showing reversibility with bronchodilator and corticosteroids groups, and in age, sex and smokers distributions. The differences in baseline FEV1 values and in the increased percentages of FEV1 values from the baseline between the bronchodilator and corticosteroids groups were calculated with Student's t test. The relationship between several parameters was evaluated using Pearson Correlation technique and the Student's t test was used to assess the significance. Probability values are two sided, and p values <0.05 were considered significant for all statistical tests.
Results
The mean (SE) and 95% CI of the baseline spirometry data of the total 60 patients studied are presented in table 1. There were 43.3% male and 56.7% female. 11.7% were between the age group 35 to 40 years, 25% between 41 to 50 years, 40% between 51 to 60 years and 23.3% between 61 to 69 years. 86.7% were smokers.
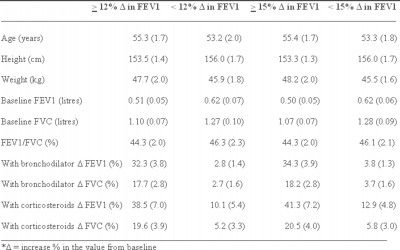
12% or more increase in FEV1 was seen in 53.3% of the patients following bronchodilator and in 60% following oral corticosteroids (p = 0.46). Similarly 15% or more increase in FEV1 was seen in 48.3% of the patients following bronchodilator and in 55% following oral corticosteroids (p = 0.47). Thus, about 48.3% to 60% of the presumed COPD patients studied had asthma and only the remaining had COPD. The male and female distributions were 40.6% and 59.4% in the asthma and 46.4% and 53.6% in the COPD groups of the 12% criteria respectively (p = 0.65). Similarly the male and female distributions were 41.4% and 58.6% in the asthma and 45.2% and 54.8% in the COPD groups of the 15 % criteria respectively (p = 0.77). The differences in age distribution were also not significant between post-bronchodilator < 12% and ≥ 12% (p = 0.556), between post-bronchodilator < 15% and ≥ 15% (p = 0.628), between post-corticosteroids < 12% and ≥ 12% (p = 0.170), between post-corticosteroids < 15% and ≥ 15% (p = 0.421) groups. Among asthma and COPD groups by the 12% post-bronchodilator criteria 84.4% and 89.3% were smokers respectively (p = 0.41) and among asthma and COPD groups by the 15% post-bronchodilator criteria 82.8% and 90.3% were smokers respectively (p = 0.28). Mean (SE) of spirometry data of asthma and COPD groups of both 12% and 15% reversibility criteria are presented in table 2.
The difference in the baseline FEV1 values was not significant between the <12% and ≥12% groups (p = 0.08), but was significant between the <15% and ≥15% groups (p = 0.047). The differences in the increased percentages of the FEV1 values from the baseline between the bronchodilator and corticosteroids groups were not significant in any groups, like <12% FEV1 (p = 0.19), ≥12% FEV1 (p = 0.44), <15% FEV1 (p = 0.07), or ≥15% FEV1 (p = 0.42) groups. The correlations with their significance values between the various parameters are presented in table 3.
Figure 1
Figure 2
Discussion
The present study highlights that in our population among 35 to 69 years-old-patients of presumed COPD, not receiving inhaled corticosteroids in spite of being symptomatic; more than half of them have asthma. The age and sex distribution and percentages of smokers were similar in both asthma and COPD groups. Almost 85% of asthma patients in the study were smokers, which could have contributed to consider them as having COPD. The fact that the asthma patients in the study population were a selected group included under the presumed diagnosis of COPD could be accounted for the high frequency of smoking in them. Smoking is also a risk factor for non-atopic asthma which is more common with increasing age. 11 Thus, history of smoking does not help to discriminate between COPD and asthma. The presence of COPD in relatively younger patients in the study is consistent with other reports from the region. 12 African Americans with emphysema were also reported to be relatively younger and having a similar degree of lung impairment as the white study populations despite smoking less. 13 Thus chronic cough, dyspnoea and wheezing in middle aged smokers could either be due to asthma or COPD.
Asthma in the elderly is increasingly reported to be frequently confused with COPD. A study of elderly patients aged 65 years or older and meeting strict criteria for asthma revealed that one in five asthmatic patients had received an improper diagnosis of COPD and a quarter of asthmatic patients did not receive any diagnosis of respiratory disease. 14 Similarly, it has been demonstrated that patients >64 years old hospitalized with a main diagnosis of asthma frequently received a diagnosis of COPD on the occasion of rehospitalization. 3 Patients with asthma, when included under COPD, are less likely to be prescribed inhaled corticosteroids. In a US study only 30% of patients aged 65 years or older who had definite asthma were taking inhaled corticosteroids. 2 Similarly 40% of patients with asthma aged 65 years or older who had experienced a recent acute exacerbation of asthma did not receive inhaled corticosteroids therapy within 90 days of discharge from their hospitalization in Canada. 1 These reports are consistent with our observation of misdiagnosis of COPD in asthmatics, but data in younger age like in our study are scarce from other parts of the world. Any prevalence study of COPD without reversible tests may, thus, erroneously include significant proportions of asthma patients. Spirometry with reversibility testing helps to minimize the confusion between asthma and COPD. But despite the recommendations of guidelines, spirometry seems to be underused by primary healthcare practitioners for the diagnosis of airway disease even in industrialized countries, 15 mainly because of budget constraints 16 . In a US report only 40% of patients with the diagnosis of COPD followed by generalists had spirometry performed. 17 Guideline for COPD in India advises that if diagnosis is doubtful patients should be ‘referred' to a specialist at the secondary care center with the facilities for spirometry. 18 An editorial of the leading medical journal in Nepal clearly states that spirometry and reversibility tests, or even peak flow meter, may not be possible in most of the local situation in the country and for all practical purpose asthma needs mostly to be diagnosed clinically. 19
The finding in the present study of more than half of the patients aged 35 to 69 years with chronic cough, dyspnoea and wheezing showing reversibility of airflow limitation needs to consider two more issues, simultaneous occurrence of and overlap of reversibility between asthma and COPD. The high incidence of concurrent respiratory disease was highlighted by a survey of over 2900 individuals in the US, where 7% was diagnosed with asthma, 11% with COPD and a further 4% met criteria for both conditions. 20 Thus, due to the high prevalence of asthma and COPD and relation of the underlying smoking habit in both, simultaneous occurrence of both the conditions may also occur. Similarly, there is overlap of reversibility between asthma and COPD. Individuals with asthma who are exposed to noxious agents, particularly cigarette smoke, may develop fixed airflow limitation and longstanding asthma on its own can lead to fixed airflow limitation. 21 On the contrary, up to 30% of patients with COPD have an increase in 15% or more in FEV1, after inhalation of a beta-agonist aerosol. 22 Thus in many patients of obstructive airway disease with chronic cough, dyspnea and wheezing, even with history of smoking, the basic issue for the clinicians may become whether to prescribe inhaled corticosteroids or not, rather than trying to distinguish them clearly as patients with asthma or COPD. Inhaled corticosteroids are the standard treatment in chronic asthma. Now inhaled corticosteroids has been recommended in COPD in different situations with FEV1 <50% predicted in current treatment guidelines. 21,23 As spirometry and reversibility testing appear not possible for significant proportions of symptomatic patients, particularly in developing countries, even for relatively younger age groups like 35 to 60 years old, guidelines to use inhaled corticosteroids along with bronchodilators also seems to be required based only on clinical presentations like functional disability and number of episodes due to COPD. Such situation is represented by the middle-aged patients of presumed COPD with history of chronic cough, dyspnoea and wheezing without receiving inhaled corticosteroids in this study.
The study has two limitations. First, post-bronchodilator FEV1 <80% of predicted value was not considered in the inclusion criteria. Reference values for FEV1 and FVC are not available for the population, with more than ten major ethnic groups with significant proportions of people living in differing altitudes, from high altitude to sea level in Nepal, a small country between India and China with cultural and ethnic influence from both 24 . Also the universally applicable reference values for FEV1 and FVC are not available. 21 But such problem may apply in research or day to day clinical practice even in industrialized countries with significant number of migrant population from the developing countries like Nepal or other bigger ones with much more varied population groups. As the FEV1 is obviously lower in the study, this limitation of not having criteria of post-bronchodilator FEV1 <80% of predicted value may not be of much relevance. Second, in the criteria for FEV1 response, though both ≥12% and ≥15% increase in FEV1 following bronchodilator or corticosteroids were considered as showing reversibility of airway and analyzed in the study, the minimum increase of 200 ml was not considered. There is no clear consensus about the methodology, variables and criteria of reversibility in subjects with airflow obstruction. 25,26,27 The three most common methods, each with its benefits and merits, of expressing bronchodilator response are per cent of the initial spirometric value, per cent of the predicted value, and absolute change. When using per cent change from baseline as the criterion, a 12-15% increase in FEV1 and/or FVC is regarded as necessary to define a meaningful response. 25 The standard textbook of medicine referred widely still does not include the criteria of increase of 200 ml in FEV1 when establishing the diagnosis of asthma by demonstrating reversibility of airway obstruction. 28
In summary, our results reveals that among 35 to 69 years-old-patients of presumed COPD not receiving inhaled corticosteroids in spite of being symptomatic, more than half of them have asthma. Age, sex and history of smoking do not help to discriminate between COPD and asthma in adults with chronic cough, dyspnoea and wheezing. Such study about misdiagnosis of COPD in asthmatics, though available in elderly in industrialized countries, is scarce in younger age and warrants further large scale controlled clinical investigation.
Role of the funding source
Nepal Health Research Council funded the study. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report
Acknowledgement
We would thank all those who participated in the study and special thank to Mr Parvin Shrestha, Statistician, for help with the statistical analyses.
Correspondence to
Manoj Nepal 151 S Bishop Ave, Apt E012 Secane, PA, 19018 manojnepal@gmail.com 01-703-861-7932