Transphyseal Spread Of Benign Conditions In Pediatric Patients: A Series Of Six Cases
V Bagaria, N Harshvardhna, D Mohan, S Sandeep
Keywords
benign tumor, chondroblastoma, infection, multi-focal osteomyelitis, transphyseal spread, tuberculosis
Citation
V Bagaria, N Harshvardhna, D Mohan, S Sandeep. Transphyseal Spread Of Benign Conditions In Pediatric Patients: A Series Of Six Cases. The Internet Journal of Orthopedic Surgery. 2004 Volume 2 Number 2.
Abstract
Epiphyseal extension of benign pathology is regarded as an infrequent occurrence. This observation has been attributed to anatomical and biochemical phenomenon unique to physeal cartilage. We report a retrospective series of six patients over a period of four years, diagnosed with benign pathologies that showed crossing of an open physeal plate by the disease. Four of these cases were infections and two were benign tumors. The patients were aged between 5 and 11 years, all of them were treated at a tertiary referral centre and followed up for a minimum period of six months to evaluate the progress of disease. We believe that this is the first time that a large series has shown that the epiphysis does not necessarily act as a barrier to spread in all benign pathologies. The findings are more than just a pathological curiosity as they alter the management and surgical procedure that needs to be performed for these conditions. The recognition of the fact that benign tumors may occasionally present with transphyseal spread will prevent unjustified radical procedures that are best reserved for aggressive malignant conditions.
Department(s) and institution(s) where work was done
Department Of Orthopaedics,
KEM Hospital,
Parel , Mumbai, India.
Introduction
Crossing the physis by primary metaphyseal localized bone tumors and osteomyelitis in child hood has rarely been observed. The physis had been traditionally been considered as a strong barrier against spread of tumors and infection. However aggressive tumors like osteogenic sarcoma were frequently reported to cross the physis1,2,3. Due to the primary noninvasive nature of infections and non-malignant tumors, there have been only isolated case reports of transphyseal spread in these group4. A series of six cases in which such a spread was seen is presented here. We believe that this is the first large series describing such occurrence in a group of benign condition.
Materials and Methods
This retrospective study includes six patients in which there was transphyseal extension of a benign pathology. These cases were identified over a period of four years in a tertiary care institute. In all the patients the physeal plate was open. The cases were examined and clinical findings recorded, a biplane radiograph of all six patients was done, three of these patients also under went MRI scanning. An orthopedic radiologist without any prior knowledge of point of the question (epiphyseal extension) was asked to review the data and form an opinion as of transphyseal involvement; Epiphyseal incongruity and areas of local bone destruction on X-rays were taken as an indicator of involvement. A tissue diagnosis was obtained in each of the cases following which appropriate course of management instituted. All the cases were followed up for an average duration of one year (shortest follow up being six months and longest follow-up was of six years). During each clinical follow-up the past clinical charts were reviewed and appropriate radiographs taken.
Illustrative Case reports
Case 1
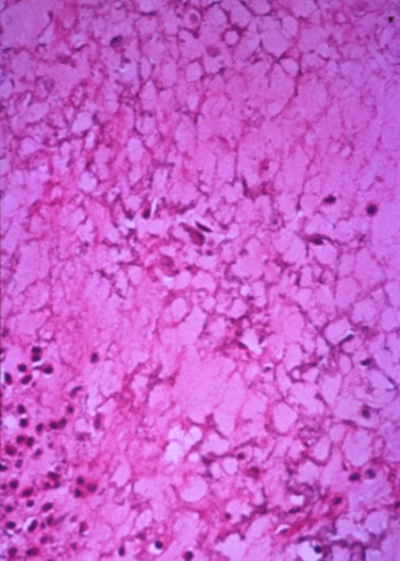
A case of chondroblastoma in an eight-year old child located in proximal humerus: the child presented with complaints of pain in the shoulder of 4 months duration, on examination there was local tenderness at upper humerus region and the shoulder range of motion was terminally restricted in all directions. Needle biopsy was done and histopathological diagnosis of chondroblastoma was established. The lesion was curetted transphyseally and the defect filled with bone graft without damaging the entire physis. At 6 month follow up there was no evidence of tumor recurrence and the defect had healed partially.
Case 2
A case of unicameral bone cyst in an 11yr old child with lesion in the proximal humerus, after obtaining a histo pathological diagnosis the lesion was treated by transphyseal curettage. On last follow up (five years), there was partial healing with sclerosis with asymptomatic shortening of humerus.
Case 3
A five-year child who presented with complaints of pain around knee joint showed a lytic lesion around distal femur, the lesion on X ray appeared to have crossed the physeal plate. The patient had constitutional symptoms in form of fever, weight loss and malaise. His blood investigation showed an increased ESR. On basis of clinical suspicion anti tubercular therapy was started. The limb was splinted in a plaster slab. The child improved clinically within six weeks, the ESR levels decreased, and following pain relief, an active range of movement was started. The lesion healed on antituberculous treatment without any surgical intervention. At two year follow-up the patient was clinically and radio logically asymptomatic. The range of motion at knee was full and painless.
Case 4
A six-year-old child presented with painful restriction of knee range of movement (ROM), on examination the child had low-grade fever, showed evidence of weight loss, and had tenderness at the proximal tibia. There was no warmth or any evidence of fluid in the knee joint. The radiographs showed a lytic lesion involving the epiphysio-metaphyseal region of proximal tibia. On blood investigations the ESR was raised and the blood count indicated a lymphocytosis. In view of these findings a provisional diagnosis of tuberculosis was made and the child was started on anti tuberculous treatment. There was sign of early improvement with decrease in pain and increased knee ROM during first two weeks; this was however followed by sudden clinical deterioration. The child presented in emergency department with severe pain and restriction of knee range of movement. The radiographs taken at that time suggested a possible involvement of the knee joint and an arthrotomy was immediately done. The lesion was left untouched. The synovial fluid was clear and did not grow any organism including myco bacteria on culture. The patient symptom rapidly improved following arthrotomy, the anti tubercular therapy was continued for one year. At one year follow up patient had no clinical signs or symptoms of the disease and the radiographs showed signs of healing of the lytic lesion with sclerosis.
Figure 10
Figure 11
Case 5
An 11-year-old boy presented with complaints of mild pain around ankle, the radiographs showed presence of lytic lesion crossing the physeal plate. A needle biopsy yielded seropurulent material, which was sent for culture. The culture report confirmed a diagnosis of tuberculosis. The patient was started on antitubercular drugs. At 8 months, follow-up the lesion patient became clinically asymptomatic but showed no signs of radiological healing. An aspiration biopsy under radiological guidance was performed in order to rule out multi drug resistance tuberculosis. There was no growth on any culture medium. The anti tubercular therapy was continued in the wake of clinical improvement and no surgical intervention was done. At one year follow up the patients is symptoms free, and the radiographs showed early signs of healing of the lytic lesion.
Figure 14
Figure 15
Case 6
A case of multifocal chronic osteomyelitis was seen in a child aged nine year with proximal humeral epiphysio metaphyseal involvement, metaphyseal involvement of lower femur and distal radius. The patient was severely under nourished and showed systemic signs of high-grade fever, severe weight loss and anorexia. He was treated with a six-week intravenous course of antibiotic (Third generation Cephalo sporin and Aminoglycoside). The child showed signs of clinical and radiological improvement after six weeks of therapy. At subsequent follow up he progressively improved in terms of pain, and ROM. The systemic symptoms disappeared and child showed weight gain and improved nutritional status at six weeks. The radiographs at one year showed almost complete healing of the lesion with child completely symptoms free. The child was lost to follow-up after one year.
Discussion
The physeal plates are thought to be a barrier for spread of infectious and neoplastic pathologies. The mechanism behind this phenomenon is still unclear. It is thought to be a consequence of production of collagen inhibitor by physis that was demonstrated in organ cell culture system5. Certain studies showed that growth plate chondrocytes secrete Transformation Growth Factor (TGF) Beta 1 that inhibited neo-angiogenesis and consequently impeded the tumor spread 6, 7.
Ghandur-Mnaymneh et al, showed, crossing of the cartilaginous plate by the malignant neoplasm (Osteosarcoma) in twelve of his fourteen patients1.Later, Panuel M et al8 in a study of 22 patients with metaphyseal primary malignant tumor (17 Osteosarcomas and 5 Ewings tumors) showed that transphyseal spread occurred in 13 cases (59%), there findings were based on preoperative MRI and correlated with pathological examination. Other series based on MRI findings and histo-pathological studies have reported a transphyseal spread rate of 75-93%9,10,11,12. Most of the studies done to study the phenomenon have indicated that the spread in malignant conditions can be attributed to neo angiogenesis seen in the tumor mass, that results in tumor vasculature crossing the physeal plate1, 13,14,15. A similar phenomenon was hypothesized to occur in infections wherein the transphyseal vessels are thought to provide a direct connection between the growth plate (physis) and the epiphyseal cartilage facilitating the spread of osteomyelitic foci in the metaphysis to epiphysis16, 17. The less common mode of approach is thought to be spread around the epiphyseal plate beneath the perichondrium and into the epiphyseal vascular channels.11, 18
The Trans physeal spread of benign conditions like infection and benign tumors have been infrequently reported in literature most often as isolated case reports4, 19, 20. This particular study is a large collection of six benign cases in which transphyseal spread occurred. These findings are not mere pathological curiosity but represent a diagnostic dilemma and alter the management plan. Unlike the more aggressive malignant tumors, many of these condition do not always require a surgical intervention, moreover surgical intervention when required needs to be less radical than those required for the malignant conditions. Three of the cases in this particular series were diagnosed early in the course of disease and resolved on conservative management in response to chemotherapy. This underlines the importance of early recognition and institution of non surgical management in some of these conditions to avoid surgical intervention that are often needed on account of delayed diagnosis and consequent disease progression. On the other hand when a surgical treatment is required, radical procedure like complete excision of the physeal plate may not always be necessary. Also a careful planning of the intervention with regards to the mode of approach to the lesion needs to be done. The risk of potential growth arrest and shortening should be anticipated and informed to the parents.
Conclusion
In conclusion we find that the occurrence of trans physeal spread in benign condition although rare is not necessarily an exception. The recognition of this fact will help expedite the diagnosis, and may also prevent unwarranted radical surgical interventions.
Correspondence to
Name: Dr. Vaibhav Bagaria Address: Department Of Orthopedics, Medical College of Wisconsin, Milwaukee, WI 3213. Phone numbers: 414-8057412 Facsimile Number: 414-8057499 E-mail address: vaibhavbagaria@rediffmail.com