Tip Apex Distance – Is It Enough To Predict Implant Failure?
N Agni, E Sellers, R Johnson, A Gray
Keywords
cutout, intramedullary hip screw, keywords: dynamic hip screw, lag screw, sliding hip screw
Citation
N Agni, E Sellers, R Johnson, A Gray. Tip Apex Distance – Is It Enough To Predict Implant Failure?. The Internet Journal of Orthopedic Surgery. 2012 Volume 19 Number 3.
Abstract
This study aimed to further establish any associations with implant cutout, in proximal femoral fractures reduced and stabilised with either a Dynamic Hip Screw (DHS) or Intramedullary Hip Screw (IMHS) device.Radiographs of 105 consecutive patients, who underwent either DHS or IMHS fixation of a proximal femoral fracture, were reviewed retrospectively. The Tip Apex Distance (TAD) was measured, using the combined AP and lateral radiograph distances. Fractures were classified according to the Muller AO classification.60 patients underwent DHS fixation and 45 patients had IMHS fixation. A TAD≥25mm was found in 9 patients in the DHS group and 6 patients in the IMHS group. There was 1 cutout in the DHS group (31-A1 type) and 4 in the IMHS group. 3 of the cutouts had a TAD≥25mm. The 4 cutouts in the IMHS group had a fracture classification of 31-A2, 31-A3 and 32-A3.1 respectively. In addition, the fractures were inadequately reduced and noted to be fixed into a varus position.A TAD<25mm would appear to be associated with a lower rate of cutout. The cutout rate in the IMHS group was higher then the DHS group. Contributing factors may have included an unstable fracture configuration and inadequate closed fracture reduction at the time of surgery.
Introduction
Hip fractures generate significant morbidity, mortality and cost within the NHS. The worldwide incidence of hip fractures has been estimated to rise from 1.26million in 1990 to 2.6million by 2025 and 4.5million by the end of 2050[1]. Based on current UK population trends, the incidence of hip fracture will likely rise from 86,000 to 120,000 by 2015[2, 3].
Peri-trochanteric fractures account for a significant proportion of these injuries. Stable fixation is essential to allow early mobilisation of patients with full weight bearing status on the affected limb. The established fixation method for peri-trochanteric fractures is a fixed angle, sliding hip screw (SHS) in conjunction with either a side plate (Dynamic Hip screw) or Intramedullary nail. The benefit of a SHS is that it allows controlled impaction of the fracture, whilst maintaining stability and a constant neck-shaft angle [4, 5].
The most frequent type of failure using this method of fixation is collapse of the femoral neck-shaft angle into a varus position. This increases the likelihood of a lag screw ‘cutout’ from the head. Failure rates of up to 23% have been reported [5]. Baumgaertner et al (1995), demonstrated multiple factors to be associated with risk of cutout [4]. These included increasing patient age, an unstable fracture pattern, inadequate reduction and the use of a high angle (150-degree) side plate. They found that the strongest predictor of failure was an increased Tip Apex distance (TAD) [4, 5]. TAD describes the position of the lag screw within the femoral head. It is the sum of the distance from the tip of the lag screw to the apex of the femoral head on both anteroposterior and lateral radiographs after correcting for magnification [6]. A TAD value of greater than 25mm is associated with increased risk of cutout [4, 5, 7, 8]. Baumgaertner et al proposed that a TAD of less than 25mm reduced this risk. Subsequent studies have not only supported this recommendation, but have suggested a TAD of less than 20mm to be ideal [4, 5, 7].
The aim of this study was to review the cutout rates of both the DHS and IMHS devices and to see if a TAD >25 mm was associated with device cutout. The study also looked to identify any other factors that may contribute to implant failure.
Patients And Methods
A retrospective review was carried out over a 21-month period using theatre logbooks at a single tertiary referral centre for orthopaedic trauma. This identified those patients who had undergone fixation of peri-trochanteric fractures with a sliding screw implant (Dynamic hip screw (Synthes) or Intramedullary Hip screw (Smith & Nephew). Patients were included who had a minimum follow up of 3 months. Patients who had incomplete clinical details or inadequate radiographs were excluded from the study.
The data collected included: relevant demographics (age and sex); classification of fracture pattern; tip apex distance measurements; follow up time and complication rates.
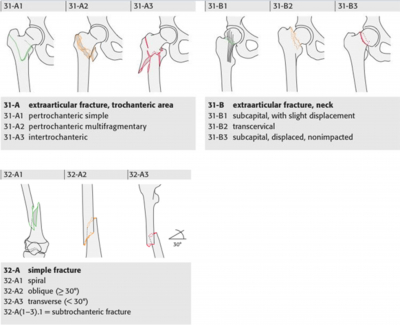
A digital based Picture Archiving and Communication (PACS) system called INFINITT PACS (INFINITT Co., Ltd. Seoul, Korea), was used to analyse radiographs. Pre-operative anteroposterior (AP) and lateral radiographs were used to correctly classify each fracture using the Müller AO Classification of Long bone fractures. Three broad groups were used to classify the data; extraarticular fracture trochanteric area (31-A); extraarticular fracture neck area (31-B); subtrochanteric diaphyseal fracture (32-A). The sub classifications relevant to this study are demonstrated in figure 1.
The Tip Apex distance was calculated using the method described by Baumgaertner et al [4]. Using intra-operative image intensifier films, measured AP and lateral radiograph distances were combined to calculate the measured TAD. One person was trained in measurement technique and used to collect all data thus minimising observational error. In order to standardise for magnification, the diameter of the lag screw on each radiograph was recorded and magnification value calculated from the known diameter. The widths of the head of the DHS and IMHS screws were 12.5mm and 12.9mm respectively. This resulted in a magnification value, which in conjunction with the measured TAD on radiograph was used to calculate the true TAD in millimetres. An illustration of this process is demonstrated in figure 2.
Collected data was entered into an excel spreadsheet. Data was analysed using direct numerical comparisons, with SPSS software package version 11.0 (SPSS Inc. Chicago, Illinois) and was expressed as a median and range. A non-parametric (Mann-Whitney) test was used to compare relevant measurements between groups. For all analyses a p value of 0.05 or less was considered to be significant.
Figure 1
Results
120 consecutive patients were identified, of which 15 were excluded due to incomplete clinical details or radiographs. Of the 105 remaining patients, 60 underwent DHS fixation and 45 IMHS fixation.
Demographic data that included age and sex was collated. Of the 105 patients, 74 were female and 31 were male. The median age was 81 (Female 84; Male 77). The minimum follow up after fixation was 3 months with (Median 5.8; Range 14) and (Median 10.9; Range 27.3) months for DHS and IMHS fixations respectively. Of the 105 fractures studied 89 were in 31-A, 6 were in 31-B and 10 patients were in 32-A. Table 1 demonstrates the relevant subgroups.
Table 2 demonstrates the TAD measurements for our entire patient cohort. There was no significant difference (p=0.96) in TAD between our two cohorts with a mean of around 18mm.
60 patients underwent DHS fixation of which 51 had a TAD < 25mm (Median 16.4; Range 16.6) and 9 had a TAD ≥ 25mm (Median 26.3; Range 7.4). There was one cutout (TAD 29.1mm) in the >25mm subgroup (31-A1 type).
45 patients underwent IMHS fixation of which 39 had a TAD of <25mm (Median 17.3; Range 15.4) and 6 had a TAD ≥25mm (Median 28.2; Range 13.1). There were 2 cutouts (TAD 23.0mm and 18.5mm) in the <25mm subgroup (31-A2 and 32-A respectively) and 2 cutouts (TAD 25.0mm and 38.1mm) in the >25mm subgroup (31-A3 and 32-A respectively). In each case the fracture had been inadequately reduced with the proximal femur in a varus position and the screw placed high in the femoral head.
Discussion
Our study demonstrated that TAD<25mm was associated with less implant failure thus reaffirming this useful predictor of screw cutout. The cutout rate in the IMHS group was higher than the DHS group, despite a comparable tip apex distance. It was also demonstrated that a significant contributor was an association with fracture mal-reduction, often seen with the more complex and less stable patterns of proximal femoral fracture (i.e. 31-A2, 31-A3 and 32-A subgroups). In these cases, the medial supporting calcar is compromised and the proximal femur predisposed to failure by collapse into a varus position.
Baumgaertner et al and Geller et al supported the conclusion that a TAD<25mm is associated with a decreased incidence of lag screw cutout after proximal femoral fracture fixation. Baumgaertner et al found that no patients with a TAD<25mm cutout and demonstrated a statistical relationship between increasing TAD and cutout, regardless of other variables related to the fracture [4]. 17% of his fracture series were also classified as having a poor reduction and that this was also related to implant failure. Geller et al demonstrated a statistically significant difference when using an intramedullary (IM) device, when comparing the outcome of TAD<25mm to TAD>25m [9]. They concluded that aiming for a TAD<25mm was just as important when using an IM device.
The optimal treatment method for unstable proximal femoral fractures remains controversial. Intramedullary devices have been shown to have biomechanical advantages over extramedullary devices. Hardy et al suggested that the IMHS device was associated with fewer complications, due to a shorter lever arm, which resulted in relatively reduced tensile force acting upon the implant [6]. However, other studies such as Bridle et al have demonstrated no difference in rates of complication, implant failure, blood loss and operative time when comparing DHS to IMHS fixations[12].
This present study suggests a greater association with implant failure using the IM device, but that this association is likely not implant related or due to a poorer mean implant position in terms of the TAD. The contributing factor to cutout would appear to be an unstable fracture configuration, with an inadequate closed fracture reduction prior to surgery. Reduced biomechanical stability of an unstable proximal femoral fracture pattern, with persistent varus malreduction prior to surgery, would appear to be associated with an increased risk of femoral head screw cutout. Walton et al showed that an IM device was suitable for unstable fracture patterns but that accurate fracture reduction and implant position were essential in order to prevent implant failure [10]. They accepted that closed reduction in unstable fracture patterns was difficult. Hak et al described an intraoperative technique of anatomical fracture reduction without varus deviation in order to decrease the cutout rate [11].
A weakness of our study may be errors in TAD measurement from radiographs. This involved the use of image intensifier radiographs taken in theatre, during surgery and subjectively determining the apex of the femoral head so that subsequent measurements could be carried out. However, Johnson et al have previously demonstrated that the TAD can be reproduced easily and accurately, from digital based systems such as Picture Archiving and Communication (PACS) [12]. They also showed that there was no difference in measurements between surgeons of different grades once instructed in the correct methodology.
An area for future study may include a prospective comparison of IM and plate SHS devices, standardising for fracture complexity pattern. A prospective comparison of fracture reduction and TAD may help determine any association with these two factors that are important in predicting future device cut-out.
Conclusion
This present study has shown that factors associated with poor outcome and increased femoral head screw cutout rates include: screw position placed ‘high in the femoral head’; a varus proximal femoral position pre-fixation; unstable fracture patterns and TAD>25mm. Cut-out rates were higher in the IMHS group, but that this is likely explained by the difficulty in achieving an adequate pre-operative fracture reduction with an associated unstable fracture pattern.