Castleman’s Disease In Childhood
G Yildirim, G Berkiten, K Turkoz
Keywords
castleman’s disease, childhood, neck
Citation
G Yildirim, G Berkiten, K Turkoz. Castleman’s Disease In Childhood. The Internet Journal of Otorhinolaryngology. 2008 Volume 10 Number 2.
Abstract
A cervical lymphadenopathy in children is considered generally as a non specific infection. But sometimes, it may be a specific infection, a malignancy or a disease of lymphoid system. Delayed diagnosis may lead to some serious results. For this reason, when there is a child with a cervical lymphadenopathy without any infection, a lot of experimental studies must be realised for the diagnosis. Castleman’s disease is a giant lymph node hyperplasia. The disease is rare in children, and neck is a very uncommon site for paediatric cases. In our case there was a painless cervical mass. After all investigations there was not any diagnosis. And after the surgery the postoperative histopathology was a Castleman’s disease.
Introduction
Castleman’s disease (giant lymph node hyperplasia, lymphnodal hamartoma) represents a unique type of lymph node hyperplasia first described by Castleman and colleagues in 1956 (1). The disease has an unsettled complexity and morbidity and has two distinct clinical expressions. Multicentric/sys temic form presents mainly with generalized lymphadenopathy and/or splenomegaly. This clinical form usually affects young adults (2). The solitary form presents as a mass located most commonly in the mediastinum but also described in the lung, axilla, mesentery, soft tissues, nasopharynx and neck (3,4).
The disease is very rare in children, and neck is a very uncommon side for involvement for pediatric cases (5,6).
Case Report
A ten year old girl was referred with an isolated, mobile, sharp bordered, firm and painless mass. The lesion was located in the left lateral part of the neck and estimated to measure 5 cm in the largest dimension.
Patient’s inquiry revealed that the mass had appeared 5 months before the presentation time. Laboratory data revealed that the patient’s hemoglobin was 13,5 g/dl., ESR was 4 mm/h, peripheral leucocyte count was 7100 per cubic millimeter, of which % 60 were neutrophils, %30 lymphocytes , %8 were monocytes and %3 were eosinophils. Total platelet account was 200000/ml. CRP was not higher than 0,5 mg/dl. Gammaglobulins were within the normal limits. Tests for tuberculosis, atypical mycobacteriae, brucellosis, toxoplasmosis, epstein barr virus, cytomegalovirus and HIV were all negative. Whole body scanning by CT showed a dense and highly vascularised mass in the left lateral side of the neck and the other body sides were normal.
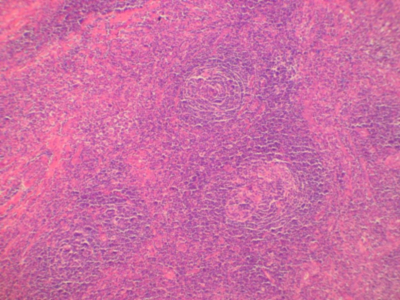
The mass was excised totally and send to the department of pathology. In routine haematoxylene and eosin slides, large follicles which showed marked vascular proliferation and hyalinization of their abnormal germinal centers were seen scattered in lymhoid tissue (Fig. I). There was a concentric layering of the lymphocytes at the periphery of the follicles (Fig. II). In hyalin centers, large cells with a vesicular nuclei were seen. These cells were evidenced as follicular dendritic cells by their immunoreactivity for CD 21 and CD35. Follicular areas were stained positive by B cell markers and interfollicular areas were positive for T cell markers. Lymph node showed positivity for both kappa and lambda chains. The diagnosis was “Castleman’s disease, hyaline vascular type”.
Figure 1
Discussion
Castleman’s disease is a unique type of lymphoproliferative disease. Its etiology is controversial and knowledge about morbidity is not settled yet. The disease has usually been reported in adults but in children the disease is rare. (6,7,8,9,10).
From the point of localization, neck is one of the rarest regions to be involved. The neck was the side of involvement only in a few children who were reported in the review of the literature by Salisbury (5,7). Grossly, lesion can be as large as 15 cm in diameter. Similar microscopic changes suggesting an early stage of the same process are sometimes seen in the adjacent lymph nodes (3). Approximately 90 % of the solitary cases are hyaline vascular subtype and remainders are plasma cell type. Hyaline vascular subtype usually doesn’t present with any systemic symptom. Symptoms like fever and weight loss; abnormal laboratory results like elevated ESR and CRP, microcytic anaemia, which consists approximately 10 % of the solitary clinical form (3). Castleman’s disease of plasma cell type can be associated with polyneuropathy, organomegaly, endocrinopathy, M-protein, skin changes and anasarca. The acronym “POEMS” is used to name this syndrome (11). The rare occurrence of Castleman’s disease, especially multicentric forms in younger ages suggests a hypothesis that environmental events play an important role in etiogenesis of Castleman’s disease and paediatric forms present an earlier form of the process (7). The diagnosis is possible only through a surgical biopsy and excision of the node with the surrounding lymph nodes is satisfactory for the cure in localized cases as in our case. All the symptoms are expected to disappear after a successful removal of the involved node. But, recurrences have been reported in adults (12). Due to her relatively poor prognosis and severity of the disease, Castleman’s disease of mixed type may be treated with combination chemotherapy consisting of cyclophosphamide, vincristine, doxorubicin, and prednisone (13). Although the clinical expression of the disease in adults is well described, further investigations are needed to clarify the pathophysiology of Castleman’s disease, especially in children.