Rectal Cancer Perforation: A Rare Complication Of Neo-Adjuvant Radiotherapy For Rectal Cancer
A Khan, Y Al Suhaibani, A Al Sharief
Keywords
diverting colostomy, neoadjuvant radiotherapy, perforation, rectal cancer
Citation
A Khan, Y Al Suhaibani, A Al Sharief. Rectal Cancer Perforation: A Rare Complication Of Neo-Adjuvant Radiotherapy For Rectal Cancer. The Internet Journal of Oncology. 2009 Volume 7 Number 2.
Abstract
Introduction
Colorectal cancer is the 3rd most common cancer in united states [1] and each year 40,000 patients are diagnosed with rectal cancer. Many reasons have been proposed which make neoadjuvant radiotherapy (RT) a beneficial tool in rectal cancer over the post operative RT. Firstly it would be given to a well vascularized region that would offer a better radiobiological environment than hypoxic postoperative tumor bed. Secondly small bowel could be displaced away from pelvic irradiation field thus decreasing potential for acute and late toxicity. Thirdly it downsizes the tumor and allows for sphincter preservation and lastly irradiated large bowel would be surgically removed and replaced by normal bowel with potential for improved function [2,3]. Refinements in the techniques of RT combined with the technique of mesorectal excision has lead to better outcomes in rectal cancer and facilitated sphincter preservation. Preoperative RT for locally advanced rectal cancer is a safe regimen, with a significant tumor down staging effect and has been established to decreases significantly, the local recurrence rate and increase the overall survival compared to postoperative RT or surgery alone [4,5] . Early complications of RT usually involve gastrointestinal tract and are generally self limited but occasionally neoadjuvant RT may lead to complications as severe as the perforation of the tumour itself which can sometimes have life threatening consequences [6].
In this paper we present a case of transmural rectal cancer perforation occurring a week after completion of a course of preoperative RT. Rectal cancer perforation as a sequel to neoadjuvant RT is an extremely rare event and after extensive literature search we were able to retrieve only six cases reported in english literature.
Case Report
A 47- year old male patient who had received a diagnosis of large bowel obstruction secondary to obstructing rectal cancer and had undergone emergency sigmoid colostomy was referred to our hospital from a peripheral hospital for further management. His past history was significant for hypertension and diabetes mellitus. Abdominal exam revealed midline scar and left sigmoid colostomy. Rest of the systemic exam was unremarkable. DRE and rigid proctosigmoidoscopy revealed an anterolateral hemicircuferentrial polypoid friable lesion 8cms from the anal verge. Biopsy confirmed the clinical diagnosis of moderately differentiated adenocarcinoma. His CBC revealed WBCs of 8.5x109.e/L, Hb of 115g/L and platelet count of 242X109.e/L. Basic metabolic panel was with in normal limits and CEA level was 12.8 µg/L. Locoregional staging with pelvic MRI revealed a transmural rectal cancer (T3) associated with mesorectal lymphadenopathy (N1) as shown in figure (Fig1). No evidence of distant spread was seen on staging CT.
Figure 1
As per the mutimodality treatment protocol the patient was planned to receive preoperative RT along with Cepacitabine. Patient received 3-D conformal RT to a total dose of 50.4 Gy in a prone position in 28 fractions. 45 Gy were given to whole pelvis including pelvic lymph nodes. 5.4Gy was given as a boost to the tumor with surrounding 2-3cms margin and mesorectum. One week after the completion of radiotherapy the patient presented to emergency room with lower abdominal pain,tenderness, fever and leucocytosis (WBCs of 14.5x109.e/L). Radiology revealed features of ileus and mild amount of free fluid. He was managed conservatively with NPO, intravenous fluids and Tazocin (Piperacillinn+tazobactum). He responded to conservative treatment but developed right lower limb deep vein thrombosis which was managed with anticoagulants. Four weeks later patient was taken for surgery after placement of retrievable suprarenal inferior vena cava filter placement.
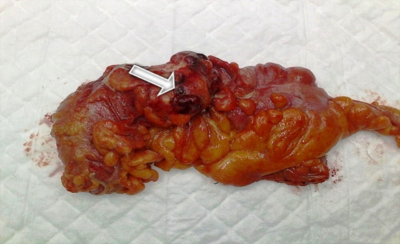
Intraoperative findings revealed tumor just above the peritoneal reflection with fibrinous flakes and few loops of intestine adherent to the loop of large gut around the tumor and small amount of loculated turbid fluid overlying the site of perforation through the centre of tumor as shown in figure (Fig 2).
Figure 2
Low anterior resection with total mesorectal excision was done. Postoperatively anticoagulants were started 48 hours after surgery. Postoperative course was characterized by a prolonged ileus. Meanwhile histopathology revealed a moderately differentiated adenocarcinoma with free proximal and distal resection margins and a radiation induced perforation through the centre of tumor ( Fig3 ).
Figure 3
16/27 lymph nodes were carrying metastasis. Finally patient recovered completely from surgery and was discharged home at 2 weeks after the retrieval of IVC filter and commencement of warfarin therapy. He underwent adjuvant chemotherapy and has no evidence of loco-regional or systemic recurrence at one year follow up.
Discussion
The well established effects of pre-operative RT in terms of reduced local recurrence and improved survival are potentially marred by side effects, which occasionally can be severe causing significant disability and thus outweighing potential benefits. Acute toxicity during the RT of rectal cancer is well known and include complications related to wound healing, gastrointestinal genitourinary and neurological complaints [7]. Marijnan et al reported acute toxicity in 26% of patients receiving radiotherapy with in three months of start of treatment. In 19% patients Grade I toxicity occurred while 7% patients experienced Grade II to III toxicity with gastrointestinal tract toxicity being most common, but only one patient developed proctitis (Grade III) [8]. Acute toxicity is usually self limited because of the mucosal involvement which has got a tremendous potential to regenerate and thus resolve with in few weeks. Adverse effects of irradiation depend up on radiation dose and irradiated volume and a strong dose volume relationship exists for the development of Grade III acute small bowel toxicity in patients receiving radiotherapy for rectal carcinoma [9]. Rolf sauer et al in their series showed grade III to IV toxicity occurring in 27% of their patients with diarrhea, dermatologic and hematological effects to be the most common. All the patients received standard 54 Gy preoperative RT. They concluded that preoperative RT was associated with reduced toxicity compared with postoperative RT [10]. On the other hand patients assigned to preoperative RT have been found to have higher incidence of septic complications [11] . Similarly Schaffer et al reported early toxicity such as dysuria, Grade I-II diarrhea and Grade II-IV diarrhea in 10,40 and 4 percent patients respectively. Grade I-II skin reactions occurred ion 44 percent of patients [12]
Rectal cancer perforation as an adverse effect of preoperative RT is an extremely rare event and extensive literature search revealed only six cases reported in english literature. Shimizu at al reported perforating rectal cancer presenting as gluteal abscess six months after radiotherapy for inoperable tumor and despite all measures patient died due to sepsis [13]. J Lee et al reported four cases of rectal cancer perforating after neoadjuvant RT, and two of the patients scummed to septicemia. All these patients were scheduled for or completed long course irradiation (54 Gy in 25 fractions) [6]. In the present case the perforation occurred after completing long course preoperative RT. The perforation in the present case could have occurred because of radiation induced lysis of tumor that was transrectal. If this is the only mechanism, it could be argued that all transrectal tumors have the potential to perforate following preoperative RT. So biological behavior of the tumor may also play an important role for such an event to occur. As the tumor grows the requirement of oxygen and nutrients overwhelms the limits of oxygen diffusion provided by host vasculature. This creates a microenvironment of hypoxia in the central part of tumor resulting in apoptosis and cell death [14]. Persistent hypoxic conditions lead to the production of VEGF which stimulates the production of proteolytic enzymes leading to degradation of basement membrane and extracellular connective tissue thus causing disintegration of central part of tumor [15]. In the presented case patient developed pelvic peritonitis and right lower limb deep vein thrombosis but was managed conservatively as he was fortunate to have a diverting colostomy constructed previously.
As short course preoperative radiotherapy (SCPRT) has been found to be safer than the long course chemoradiation [10,16] It could be conceived that tumor perforation can be reduced by SCPRT regimen of 25 Gy in five fractions. Martel et al reported a case of rectal cancer perforation occurring after patient received a short course of radiotherapy (25 Gy in 5 fractions). Patient developed peritonitis and required an operation to save life [17].
Despite the present report and isolated previous reports, perforation or no perforation of rectal cancer following neoadjuvant RT remains enigmatic. And more studies for careful tumor assessment, biological behavior of tumor and RT planning may be needed to solve this enigma. But the utmost important issue in such cases, which will help to reduce the mortality is the construction of prophylactic colostomy particularly for tumors above peritoneal reflection.
Conclusion
Rectal cancer perforation, albeit rare, is a dangerous early complication of neo-adjuvant RT for transmural rectal cancer which may be worthy of consideration and discussion when commencing treatment. Role of prophylactic diverting colostomy in such patients with cancer above peritoneal reflection remains an open question which needs to be redressed by further studies.
Acknowledgements
We express our sincere thanks to the patient for giving his consent to publish this report. Our sincere thanks to Dr. Wasim for helping us to look into radiotherapy related issues.