Giant Cell Tumour Of Bone: Risk Factors For Recurrence
M U Christmas
Citation
M U Christmas. Giant Cell Tumour Of Bone: Risk Factors For Recurrence. The Internet Journal of Oncology. 2022 Volume 17 Number 1.
DOI: 10.5580/IJO.56262
Abstract
The treatment of giant cell tumors (GCTs) of bone remains a difficult problem as the best treatment option for these benign, sometimes locally aggressive tumors remains controversial. Surgical options include intralesional excision (curettage) or en bloc resection of the tumor. Most surgeons agree that the major factor in the success of local tumor control is how thoroughly the tumor is excised and for this reason the surgeon needs to strike a balance during treatment between reducing the incidence of local recurrence while preserving maximal function. Current literature suggests that intralesional curettage strikes the best balance between controlling disease and preserving optimum function in the majority of the cases though there may be occasions where the extent of the disease mandates resection to ensure adequate disease clearance. Though curettage is the most attractive method because it seeks to preserve autologous structures, architecture and native joint cartilage, this benign lesion is well known for its great propensity for local recurrence. The question still remains; are there modifiable and unmodifiable risk factors identified in influencing the recurrence of these lesions? A case of delayed recurrence is discussed and the literature is reviewed with a focus on the identifiable risk factors for recurrence of GCTs in bone.
CASE REPORT
A thirty-one-year old female presented to the Orthopaedic Department with a four-week history of mild pain and swelling to the right knee. The pain was intermittent but had worsened rapidly, and was now felt at rest. She also began experiencing night pain. There was no history of trauma reported and there were no constitutional symptoms.
Nine years previously, she had been treated for a GCT to the right distal femur, with meticulous intralesional curettage using a high-speed burr, a local adjuvant (hydrogen peroxide) and bone grafting with cancellous chips. Themedial cortical window created had been refashioned with bone cement plug and the periosteum and fascia were closed over this cement plug. She was compliant with postoperative rehabilitation but was lost to follow-up after two years.
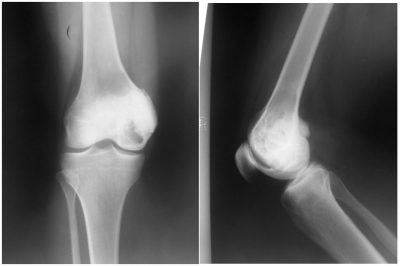
Examination revealed an adequately nourished adult female. She had an antalgic gait and ambulated with the assistance of axillary crutches, partial weight bearing on the affected limb.A surgical scar was noted on the right distal medial thigh in keeping with previous surgery. There was mild quadriceps wasting with a mildly tender swelling to the medial aspect of the distal thigh. Active range of motion of the knee was limited by pain to 0-120°.No ligamentous laxity was demonstrated. The neurovascular status of the limb was normal. She was investigated with plain radiographs and magnetic resonance imaging of the right knee (figures 1 and 2).
Figure 1
Figure 2
Three weeks after presentation, she underwent a repeat extended curettage. An incision was made on the distal medial thigh, excising the previous scar. The vastus medialis was elevated and the cortex accessed anterior to the medial collateral ligament (figure 3A). The cement plug was removed by drilling bone around its periphery (figure 3B). tumor was seen adherent to the plug’s undersurface. The cavity was curetted, power-burred, then irrigated with hydrogen peroxide and normal saline (figure 3C). Forty-five milliliters of cancellous bone allograft was impacted into the cavity. Cortical struts were used to buttress the outer cavity and bone putty packed into any remaining defects (figure 3D). The wound was closed in layers.
Figure 3
Immediately post-operatively, the right lower limb was immobilized in an above knee, Plaster of Paris back slab that was later replaced by a hinged knee brace at two weeks. Histopathologic findings confirmed recurrence of the Giant Cell Tumors. She progressed through crutch walking to independent ambulation over a six-month period. Radiographs done at the six month follow up showed no radiographic evidence of recurrence and confirmed incorporation of the bone graft. She regained full knee extension and flexion however there was no hyperextension when compared to seven degrees hyperextension on the contralateral knee. At one-year follow-up, she was fully functional with respect to her daily activities of daily living and complained of occasional mild pain to the surgical site.
DISCUSSION
The reported incidence of GCT of bone in Western countries is about 5% of all skeletal tumors and approximately 22% of all benign bone tumors (1-4). A higher incidence of GCT compared to the reported incidences for other regions around the world has been reported in the Indian subcontinent population and the South East Asia region (5-9). Many surgeons treat giant cell tumor of bone (GCT) with intralesional curettage. Wide resection is reserved for extensive bone destruction where joint preservation is impossible or when expendable sites are affected. This type of tumor of bone has a well-known propensity for local recurrence after surgical treatment. Local recurrences appear to be related to the surgical margin and are clinically characterized by pain and radiologically by progressive lysis of the bone graft or the adjacent cancellous bone. If the option of treatment is curettage with cementation, lysis or failed development of the sclerotic rim between the cement and cancellous bone may suggest recurrence (10). Current recurrence rates between 10-20% with meticulous curettage and extension of tumor removal using mechanized burrs and adjuvant therapy are a vast improvement on the historically reported recurrence rates of 50-65% with curettage alone (1, 2, 11-16). However, risk factors for recurrence still pose a problem and thus the best treatment of these tumors remains controversial.
Saika et al retrospectively studied 124 cases of histologically proven GCT of bone in an Indian population, treated at their institution and found that though their incidence of GCT was higher than that of the Western world, their overall recurrence rate of 10.3% was comparable to those reported in the available literature.(5) Similarly in a retrospective analysis of 621 Chinese patients in a single institution, thirty-five (12.4%) of the 283 patients with a primary giant cell tumor developed a local recurrence after a median of nineteen months (9). Ethnicity, therefore, appears to have no significant influence on recurrence rates and cannot be seen as a risk factor.
Klenke et al retrospectively evaluated the recurrence-free survival after surgical treatment of GCT in 118 patients between 1985 and 2005 to determine the influence of demographic factors on the risk of recurrence. Among the disease-related and demographic factors analyzed for their impact on recurrence, they found that age at the time of diagnosis independently predicted recurrence regardless of the status of the disease and the aggressiveness of the chosen treatment. The recurrence rate decreased as the patient’s age increased. Subgroup analysis revealed patients 25 years and younger at diagnosis had the greatest hazard of local recurrence (17). The greater risk of young patients having recurrence develop has been reported in the past and is thought to be associated with increased bone turnover in young people (13). On the contrary, when Niu et al analyzed age as it relates to recurrence-free survival, they found that age did not have a significant effect on survival in their population (9). Gender was not found to have any influence on the rate of recurrence of GCT of bone (9, 16, 17). Similarly, the presence or absence of a pathological fracture in the involved location was not found to have a significant effect on local recurrence (9, 16).
The location of the tumor has been indicated in the past to influence local recurrence. Some authors reported that the recurrence rate varied depending on the tumor site (18, 19). Vander Griend et al pointed out that giant cell tumors in the distal part of the radius were particularly aggressive. In their series, 74% (seventeen) of twenty-three patients received tumor resection and an additional patient underwent amputation due to recurrence (20). A higher rate of local recurrence among distal radius lesions treated with curettage compared to lesions in other anatomic locations has been described (21, 22). Kremen et al retrospectively reviewed 230 patients with giant cell tumor of bone treated from over a thirty year period and found that their local recurrence rate in distal radius lesions treated with curettage and adjuvant phenol cautery was much lower by comparison (23). The authors believed that much of this discrepancy came from differences in the treatment modalities utilized to treat these particularly aggressive tumors rather than the location of the tumor itself being a risk of recurrence (23).
The Campanacci classification is often used to grade these tumors radiologically as Grades I, II and III. Grade I is described as well-defined tumor with a radio-opaque rim, Grade II as well-defined margins with moderately expanded but intact cortex and no radio-opaque rim and Grade III as ill-defined margins with soft tissue mass (1). Grade I is rare and represents a quiescent form in which the involvement of cortical bone is minimal. Grade II is the most common type accounting for more than seventy percent of all GCTs of bone, and shows a thin and moderately bulging cortical shell, whereas grade III tumor severely destroys cortical bone and infiltrates into soft tissue and/or joint space (1). Even though the increasing grade from I to III does not appear to be a reflection of the biologic aggressiveness of the tumor, Rock, Saikia et al, Prosser et al and O’Donnell et al and others have all reported a correlation of recurrence with Grade of these tumors documenting an increased rate of local recurrence of grade III lesions (2, 5, 21, 24, 25). However, the rate of recurrence-free outcomes was found to be insignificant by other authors, between Campanacci grade-I and II tumors and grade-III tumors and had no significant influence on the recurrence rate (16, 26). In fact, one author differed in that grade III was associated with a significantly lower local recurrence rate compared with grade II (9). The grade of tumor as a risk factor of recurrence is still therefore somewhat controversial. The difference in outcomes with respect to the grade might be explained by the choice of operation, since a higher percentage of the grade III are subjected to resections rather than curettage and the difficulty experienced in achieving complete clearance once the tumor has breached its normal anatomic boundaries and extended into soft tissue. The recurrence of GCT often occurs within twelve to twenty-four months. The index case showed recurrence some seven years after curettage of the primary lesion. Though the majority of recurrences usually occur within the first two years, late recurrences are known and long-term surveillance is recommended in these patients (27, 28),
Treatment is a balance between oncological adequacy and functional utility of the limb. The current literature suggests that intralesional curettage with or without adjuvants strikes the best balance in achieving these goals (25, 29, 30). However, there is no consensus in the literature as to whether intralesional curettage carries a higher recurrence rate than wide excision (1, 13, 16, 23, 31, 32). Kremen et al retrospectively reviewed the records of 230 patients with giant cell tumor of bone, stratifying them by primary versus recurrent disease and by surgical treatment and they found a decreased recurrence rate in patients treated with wide excision (23). Similarly, Klenke et al found that out of the twenty-five patients (21%) from a patient population of one hundred and eighteen who had a local recurrence, one of the patients treated with wide resection had local recurrence while twenty-four patients (25%) treated with intralesional surgery experienced local recurrence (17). Analyzing the hazard ratios associated with recurrence, they found that intralesional surgery had a greater risk of local recurrence compared with wide resection (17). Becker et al in their review of 298 patients showed that in comparison with intralesional procedures, wide resections achieved a significant reduction in the hazard of a recurrence (16). Many of these authors however, included in their studies multiple surgeons, which would introduce potentially considerable variability in surgical techniques (1, 16, 32).
The surgeon has several options available of filling the defect after intralesional curettage. These include autograft bone, allograft bone, an artificial bone graft substitute, or polymethylmethacrylate (PMMA) bone cement (33-35). Bone graft has the theoretical advantage of restoring normal biomechanics to the joint surface to prevent future degenerative joint disease and restoring bone stock. However, two main disadvantages to its use include an extended time for joint protection to prevent a pathological fracture and the difficulty in differentiating tumor recurrence from graft resorption. These disadvantages may be overcome with the use of bone cement as a filling agent (3). In addition, the exothermic reaction of PMMA generates local hyperthermia, which induces necrosis of any remaining neoplastic tissue without causing any major local complication. It provides immediate support and allows for intensive curettage even in the case of large tumor cavities. The additional advantages of low cost, ease of use, lack of donor-site morbidity, elimination of the risk of transmission of disease associated with allograft make PMMA a very encouraging option. It also facilitates the radiographic detection of local recurrence earlier and easier (30). The use of polymethylmethacrylate as an adjuvant is reported to significantly reduce the recurrence rate following intralesional treatment of benign GCTs (16, 25).
Klenke et al in their analysis of surgical management of recurrent GCTs of long bones found that the use of PMMA instead of bone grafting was associated with a decreased risk of tumor recurrence (36). Similar observations were reported for a series of sixty-six patients with recurrent GCTs of the axial skeleton and the extremities (37). Blackley et al prospectively analyzed fifty-nine patients who had a giant-cell tumor of a long bone to determine the rate of local recurrence after treatment with curettage with use of a high-speed burr and reconstruction with autogenous bone graft with or without allograft bone. The twelve percent rate of local recurrence (seven of fifty-nine patients) that resulted appeared comparable with the clinical results reported after the use of chemical adjuvants and cement. They attributed this improvement in part to the extensive use of a high-speed burr. The authors concluded that their study suggested the risk of local recurrence after curettage with a high-speed burr and reconstruction with autogenous graft with or without allograft bone is similar to that observed after use of cement and other adjuvant treatment (34). With respect to curettage and bone cement, the reported rate of local recurrence by O’Donnell et al using curettage and bone cement was 33.3% that decreased to 16.6% when a mechanical burr was used, so they recommend using the burr at the end of all procedures (21). Balke et al also reported high-speed burring plus use of PMMA decreased the rerecurrence rate compared with that of intralesional curettage without any additive therapy. PMMA void filling without high-speed burring showed a tendency toward increased recurrence rates (19).
Once the decision has been made to treat with intralesional therapy, the surgeon then decides whether to use adjuvant therapy to eliminate microscopic remnants of the tumor from the cavity after curettage. Additional adjuvant treatment of the bone bed with hydrogen peroxide, liquid nitrogen or phenol after removal of the tumor has been advocated to decrease the risk of local recurrence when cement is used alone (16, 19, 38, 39). However differing opinions pertaining to the use of adjuvants for extension of curettage is one of those issues that offer topics for eternal debate. Phenol may be advocated as a safer agent than liquid nitrogen for adjuvant therapy because of its reduced depth of penetration with respect to its effective zone of osteonecrosis. Becker et al found the rate of recurrence-free outcomes of between 73% and 85% in patients treated with adjuvants in their retrospective study. Without the use of adjuvants, intralesional treatment resulted in a significantly lower recurrence-free outcome of 51% (16). The authors also found that there was no significant difference among the types of adjuvant therapy regarding the rate of local recurrence, although, as a whole, the group treated with adjuvant therapy had a significant reduction when compared with the group that did not receive adjuvant therapy (16). The study by Trieb et al demonstrated that local recurrence rate of giant cell tumors located in long bones treated with or without phenol was similar (40).
A multicentric retrospective study of giant cell tumor of bone was conducted among Canadian surgeons using 186 patients with GCTs of bone. The authors found that patients with primary tumors treated with curettage had a 10% recurrence rate. For recurrent lesions treated by curettage, the recurrence rate was 35% suggesting that recurrence is a risk factor for re-recurrence (32). Contrary to the results of the Canadian multicenter study, another study including 384 surgical procedures, involving 256 primary and 128 recurrent tumors, a significant difference was not found in the rate of recurrence of recurrent tumors compared with the rate for primary tumors (16). When the type of procedure performed on each group was analyzed, the use of wide resections did not differ substantially between the two groups. When treated intralesionally without adjuvants, recurrent tumors had a superior rate of recurrence-free outcomes (61%) compared with primary tumors that had been treated the same way (45%). The authors assume that the surgeon’s lack of thoroughness when curetting the tumor cavity was responsible for the poor results in the primary cases, and his or her awareness of dealing with a recurrent tumor apparently led to more aggressive surgical treatment of recurrent tumors (16).
CONCLUSION
Awareness of the typical high risk of recurrence of giant cell tumors is an important factor in the treatment of these tumors. Given the lack of randomized controlled trials, there are no conclusive data in the literature to guide clinicians as to how to appropriately stratify patients to determine which subset of patients may be at higher risk of local recurrence, emphasizing the need for a thorough curettage if chosen as the treatment option. The current literature strongly suggests that the surgical treatment of resection decreases the risk of recurrence when compared to curettage. There is conflicting evidence in the literature however, regarding local recurrence among patients stratified by age, grade, location (distal radius lesions), presence of pathological fracture, use of adjuvants, use of mechanical high speed burr or primary versus recurrent disease. The success of this method of treatment however, is related primarily to how thoroughly the tumor is removed. It is important that we recognize that adjuvant agents cannot prevent recurrence if the tumor has not been adequately removed. Therefore, adequate removal of the tumor seems to be more an important predictive factor for the successful outcome of primary surgery. The key to ensuring an adequate curettage with complete removal of tumor is obtaining adequate exposure of the lesion. This is achieved by making a large cortical window, which is necessary for appropriate visualization of the entire tumor cavity to obtain extensive curettage. A high power burr to break the bony ridges helps to extend the curettage and is now being strongly recommended. It is believed therefore from the existing literature that meticulous intralesional curettage with extended tumor removal using mechanized burr and adjuvant therapy can result in a comparable low risk of recurrence in the treatment of most giant-cell tumors of bone, leaving en bloc excision for the more aggressive lesions and lesions found in expendable bones.