Intracranial Spread Of Intramedullary A Spinal Cord Ependymoma
S Rasras, A Soltani, R ilkhchi, M Panahbekhoda, M Mashari, S Fallahpour
Keywords
ependymoma, radiotherapy, seeding, spinal tumor
Citation
S Rasras, A Soltani, R ilkhchi, M Panahbekhoda, M Mashari, S Fallahpour. Intracranial Spread Of Intramedullary A Spinal Cord Ependymoma. The Internet Journal of Neurosurgery. 2009 Volume 7 Number 2.
Abstract
Spinal dissemination of intracranial ependymomas through cerebrospinal pathway is not rare and has been reported in approximately 10% of the cases. However, the reverse is an uncommon phenomenon. We report one case that was initially treated for spinal ependymoma but later presented with intracranial metastasis.
Introduction
Ependymomas are an uncommon group of glial tumors that typically arise within or adjacent to the ependymal lining of the ventricular system (1). Ependymomas occasionally occur within the brain parenchyma or outside the central nervous system (CNS). The spread of ependymoma from brain to spinal canal occurs in approximately 10% of all cases (2). Dissemination of the neoplastic cells within the ventricular cavity is thought to be facilitated by the active circulation of the cerebrospinal fluid (CSF) throughout the neuraxis, coupled with the effect of gravity (3). However, the reverse is an uncommon phenomenon (4). We report a young man with intracranially disseminated spinal ependymoma.
Case report
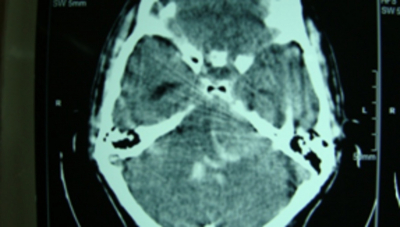
A 32-year-old male presented with sudden decrease in his level of consciousness and seizures. Admitting GCS was 6/15. anisocoric (R=2, L=4mm) mild right hemiparesis 3/5 and bilateral upward plantar reflexes was present. He had a medical history of spinal malignant ependymoma at the T12-L1-L2 level that surgically total removed 2 years ago and then radiotherapy was done. One year later treated with conventional radiotherapy 5600 cGY for seeding in L2-L3 level without recurrence in tumor bed (Fig. 1). Brain CT scan showed a cerebellopontine angle mass with IVH mild hydrocephalus (Fig. 2). The patient underwent an emergency EVD and then VP-shunt after the surgery pupils was isocoria and GCS=7/15 and one day after shunt the mass was operated and near total excision of cerebellopontine angle lesion was done. After surgery hemiparesis was recovered but otherwise no change in patient’s GCS was seen. He received a course of chemotherapy. In the follow up a tracheostomy was done and with physiotherapy and GCS of 9/15 the patient was discharged. A grossly yellowish brown tumor had been found during the operation and microscopically cluster of atypical cells with hyperchromatic nucleus and foci of papillary like structures with fibrovascular core that lined by epithelial like cells with few necrosis and mitotic activity compatible with malignant ependymoma was found.(fig.3)
Figure 1
Figure 2
Discussion
Spinal cord ependymomas comprise less than 2% of all central nervous system neoplasms, 15% of spinal cord tumors, and up to 60% spinal cord gliomas (5). Surgery is the treatment of choice for intramedullary ependymomas. Total excision of the tumor, especially in low-grade spinal ependymomas, leads to excellent results (6). However, incompletely resected high-grade spinal ependymomas have a dismal prognosis. Postoperative radiation therapy has improved the outlook for these patients significantly. It has played an important role in local control and prolonging life by increasing the 5-year survival estimates three-fold (7).
Spread of intracranial tumors into the spinal canal, especially high grade ones, is a well-known entity. In spinal ependymoma series, most of treatment failures have been reported to be local, whereas distant metastases and dissemination through CSF have been rarely documented (4, 7, and 8). Rezai et al reported that 11.4% of all intracranial ependymoma cases were disseminated into the central nervous system (2). Whitaker et al reviewed 14 spinal ependymoma series from the literature and calculated 5.8% incidence of cranial relapse in 259 patients (6). Waldoron et al reported 2 patients out of 59 who relapsed within brain (3).
We consider our patient as intracranial dissemination of spinal ependymoma. In this case, the brain CT scan (Fig. 2) revealed a tumoral mass in the cerebellopontine angle which was previously normal (Fig. 3). Considering the period of symptoms’ progression, it is unlikely that the primary lesion was intracranial, or that the lesions were multifocal initially.
There are certain treatment options in ependymomas cases. Although, radiotherapy was an effective measure in our case but altered level of consciousness and brain edema urged us to perform surgery. Emergency near total excision of cerebellopontine angle mass and intracranial decompression performed.
Analysis of 140 patients performed by Rezai et al (2) revealed that relatively younger patients were at higher risk for dissemination of the primary tumor during their clinical course. In previous reports, the patients with intracranial tumors showing spinal cord dissemination were generally young with an age range from 5 to 48 years and median was 16.8 years. Although, multiple operations on intramedullary spinal cord tumors have been proposed as a risk factor for spinal cord and cranial dissemination, it is difficult to assess the association statistically (3). But, in this patient total excision of initial tumor and one single operation before the dissemination is not consistent with this possible risk factor.
There are conflicting data in the literature regarding the correlation between ependymoma histology and clinical prognosis. It has been shown that high grade ependymomas disseminate more commonly through the CNS.
Whitaker et al (6) reported 3 cases of intracranially disseminated ependymoma. Two of them received craniospinal irradiation due to high-grade tumor. Shaw et al (8) reported one adult patient with grade 3 disease who disseminated intracranially, out of 22 patients with spinal ependymoma. In other series, Waldron et al (4) reported two (2/59) intracranial failures, both with anaplastic tumors. Our case, being high-grad, is consistent with previous reports.
In conclusion, although it is rare, but it should be noted and kept in mind that spinal ependymoma may disseminate into the cranium especially in high risk cases. A complete radiographic evaluation of the entire neuraxis should be performed in the initial work-up of these cases and the treatment should be planned accordingly.