Gas Gangrene Of The Liver With Acute Liver Failure And Septic Shock Syndrome Caused By Clostridium Perfringens
H Bergert, T Illert, J Pyrc, K Friedrich, D Ockert
Keywords
clostridium perfringens, liver failure, multiple organ failure, sepsis
Citation
H Bergert, T Illert, J Pyrc, K Friedrich, D Ockert. Gas Gangrene Of The Liver With Acute Liver Failure And Septic Shock Syndrome Caused By Clostridium Perfringens. The Internet Journal of Internal Medicine. 2002 Volume 4 Number 1.
Abstract
Since the first description of an internal organic gas gangrene by Fraenkel in 1889, only a few cases of acute organ failure following a clostridium perfringens infection have been described in the medical literature. The isolated clostridium perfringens infection with a consecutive septic syndrome belongs to the extremely rare clinical pictures. An eventually consecutive multiple organ failure has in general a very high mortality rate.
We report about 58 year-old male patient with fulminant spongious liver failure following a clostridium perfringens infection. Despite all intensive care measures taken including an interventional pigtail catheterizing, the physical condition of the patient deteriorated rapidly and took a lethal outcome. In this case report we describe the symptoms of isolated liver gas gangrene abscess as well as the taken treatment measures in comparison with the medical literature.
Clinical Course
The 58-year-old male patient was acutely admitted to our emergency unit because of subfebrile temperature and diffuse abdominal tenderness and pain mainly in the right upper abdomen since two weeks. One year before the patient had undergone a Whipple's procedure in our hospital because of an pT4, N1-Adenocarcinoma of the Vater's papilla. The postoperative course was at that time besides an anastomositis and the subsequent functional stomach disorder, unobtrusive.
One year later, the patient was admitted again at a regional hospital while complaining about upper abdominal pain, unclear fever with shudder and general wearness. The undertaken diagnostic measures including gastroscopy, ultrasonography and abdominal CT-scan showed only an urinary tract infection, but no significant cause which could account for his deteriorating general health condition. With increasing lab values of infection a blood culture, which revealed an escherichia coli infection, was taken and the patient was treated in accordance to the microbiological results with ciprofloxacin. Due to the rapid aggravation of the health condition the patient was finally transferred to our hospital.
At admission we registered a diffuse tenderness of the abdomen without any bowel sounds and a distinct pain in the upper abdomen. There were no abdominal guarding or peritonitis signs. The blood analysis showed a marked increase of the liver enzymes (ALT: 2769 IU/L, AST: 10561 IU/L, total bilirubin: 131,7umol/L), of the inflammatory lab values (WBC: 34,1Gpt/L, C-reactive protein: 52mg/L) and diffuse coagulation dysfunction (PT: 14%, PTT: 109s, ATIII: 48%) combined with a hypotonic cardiovascular state. The abdominal ultrasonography was not reliable because of the diffuse gas concentration in the upper abdomen. The chest X-ray showed a free air sickle between the diaphragm and the liver (Fig. 1). During an abdominal CT-scan a percutaneous pigtail catheter was inserted into an extensive gas-producing abscess of the liver (Fig. 2). A brownish, nearly scentless fluid mixed with gas was drained by this procedure. A few hours later, the patient presented the clinical symptoms of a multiple organ failure. Despite maximal intensive care treatment with kidney substitution therapy, substitution of coagulation factors and catecholamins, the patient died 24 hours after admission. The patient never reached an operating state. The microbiological presence of clostridium perfringens was revealed in the drainage fluid.
Pathophysiology and Autopsy
Clostridium are ubiquitous in the nature. In the human being they can be found in the stomach, the small intestine, the bile ducts and the female genital tract.
The incubation time of a primary isolated gas gangrene in a deep contaminated wound covers between 1 and 3 days. Initially the tissue necrosis takes place directly in the wound and then spreads to the neighbouring tissues and organs (5, 11). Clostridium perfringens produces a variety of pathogenic factors with local and systemic effects. The alpha-toxine ranks among the strongest factors with its hemolytic action. The other produced factors act primarily on the vascular endothelium causing a capillary leakage. This induces a liquid and electrolytes shift causing cardiovascular reactions such as hypotone blood pressure, bradycardia and finally a shock syndrome.
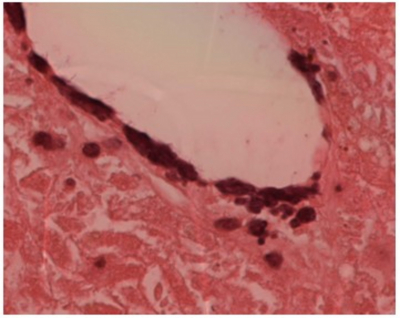
Depending on the localization, the isolated organic gas gangrene manifests itself initially with systemic inflammatory reactions and a breakdown of the specific infected organ. The next step is a spreading to the neighbouring tissues and organs and a generalized gas gangrene often leads to death, if intensive therapeutic measures are not taken immediately (1, 6). The autopsy of the here presented case showed a diffuse gas gangrene of the liver with total necrosis of the right liver lobe. This one showed a spongious alteration of the parenchyma with a dystrophic calcification of the necrosed hepatocytes (Fig. 3 and 4).
Besides, we observed a fibrinoid perihepatitis with subcapsular liver haematoma, a phlegmoneous inflammation of the diaphragm, a fibrinoid-pyogenic pleuritis with haematoma of both bases of the lung and a pyogenic gas gangrene of the fat tissue of the right colon flexura with microbiological confirmed presence of clostridium perfringens (Fig. 4). Further, we noticed a retroperitoneal lymph node infiltration of an adenocarcinoma of the Vater's papilla, primarily R1 resected, with a partly nodal and partly hard tumor infiltration into the soft tissue of the liver recess (porta hepatis) and a distinct infiltration with stenosis of the proper hepatic artery and portal vein.
Figure 3
Discussion
In 1861 Louis Pasteur characterized the genus clostridium for the first time and Fraenkel presented in 1889 the first case report of an organic gas gangrene of a 35 year-old-woman with pyogenic stomach inflammation. Since that time there have been only a few isolated case reports about this rare disease (1, 3, 7, 14, 15, 21).
Up to the middle of the last century, the generalized gas gangrene was often a consequence of soil contaminated war wounds, and took mostly a lethal end (5, 10, 11).
Today we distinguish three kinds of gas gangrene: the posttraumatic, the postoperative and the spontaneous form, while this last form is often combined with a malignant or immunsupressive primary disease (1, 4, 8, 14, 17).
From their investigation performed in the 1980's, Schmauss as well as Nier et al showed that organic gas gangrenes after an abdominal intervention occurred in a non negligible percentage of cases and that the death rate was substantially higher than after soft tissue infection (13, 18,). Those reports described about 22 infections with clostridium perfringens with a mortality of 91%.
From 15 patients with clostridium perfringens infection after visceral operation Nier et al described a mortality rate of 53% (13). Beckerhinn et al reported of some gas gangrene mediastinitis after Boerhaave-syndrom where the initial infection sign were by no means typical of a clostridium infection (3). As in our here reported case developed rapidly a multiple organ failure.
Comparing the mortality rate of liver abscess producing anaerobic and aerobic germs, one cannot find significant differences (2, 9, 16). But anaerobic infections are poor of symptoms and their progress is faster, which leaves less time for a therapeutic reaction (6,12). Here a high dosis of penicillin (20 to 40 million units a day) in combination with clindamicin and metronidazol seems to be an effective drug treatment (20). In our presented case, the primary malignant disease of Vater's papilla and the consecutive tumor resection in form of a Whipple's procedure with a hepatico-jejunostomy (Roux-Y) reconstruction, was a decisive cause of the gas gangrene in the liver. The origin probably is a biliar germ ascension. In the literature, some descriptions of a higher incidence compared to the normal population of liver abscesses after biliodigestive anastomosis or endoscopic interventions such as papillotomy or stent implantation following a hepatobiliary tumor may be found (7). Besides the germ ascension a tumor induced immunosuppressive condition may also have some influence. Therefore those patients may profit from a prophylactic antibiosis whenever a palliative intervention takes place or on the slightest clinic suspicion of an abscess.
Correspondence to
Hendrik Bergert, M.D. Department for Visceral-,Thoracic- and Vascular Surgery University Hospital Dresden Fetscherstraße 74 01307 Dresden (Germany) Tel. +49 351 4582863, Fax +493514585751, E-Mail hendrikbergert@web.de