Rectus Sheath Haematoma Mimicking An Ovarian Mass
E Thia, J Low, H Wee
Citation
E Thia, J Low, H Wee. Rectus Sheath Haematoma Mimicking An Ovarian Mass. The Internet Journal of Gynecology and Obstetrics. 2002 Volume 2 Number 1.
Abstract
Rectus sheath haematoma (RSH) is an unusual cause of a painful abdominal mass. We report a case of rectus sheath haematoma that was referred to KK Women's and Children's Hospital, Singapore because initial radiological investigations suggested an ovarian tumour.
Case Report
A 41year old woman, para 3, presented to her general practitioner complaining of left iliac fossa pain for 2 weeks. There was no history of trauma, nausea, vomiting, fever or chills. Co-incidentally, she developed a cough 2 weeks before her presentation. There was no other significant medical history of note. Pelvic ultrasound showed an elongated tubular structure measuring 8cm by 3cm located in the left adnexa anteriorly. It was cystic with non-specific internal echoes with slight thickening of the wall at some parts. The impression was of an ovarian cyst containing some non-specific internal echoes or a hydrosalpinx. She was referred to KK Women's and Children's Hospital for further management.
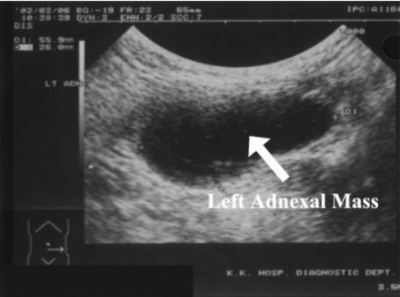
Physical examination revealed a vague mass over the left iliac fossa with slight skin discoloration over the area. Bimanual vaginal examination demonstrated an 8cm left adnexal mass, which was slightly tender. Ovarian tumour markers performed were within normal limits: Ca125 5.5 U/ml, HCG <2 IU/L, FP 4.1 ug/L and CEA <0.5 ug/L. Her haemoglobin was 11.1 g/dl and total white count was 7.57x109/L. A repeat pelvic ultrasound scan showed a left adnexal cystic tubular structure measuring 5.6 by 4.4 by 2.6cm
A laparotomy was performed for a suspected ovarian tumour. Intraoperatively, an 8 cm by 4cm haematoma that was encapsulated between the left rectus muscle and preperitoneal fascia was found. This was arising from a rupture of the left inferior epigastric vein. The haematoma was resected and the ruptured left inferior epigastric vessels were ligated
Discussion
Rectus sheath haematoma is a well-described entity with a reported incidence of misdiagnosis as high as 93%(4). RSH occurs 2 to 3 times more often in women than men(1,4). The higher incidence in women is presumably due to decreased muscle mass as compared with men(4).
RSH may be due to trauma, an underlying disease blood dyscrasia, degenerative muscular disease, anticoagulation therapy and pregnancy, or spontaneous rupture of the epigastric vessels or the rectus muscle(3). Acute paroxysmal coughing (as in this case), asthmatic attacks, bronchitis or influenza was the precipitating event in 56% of cases in one report(3).
RSH usually occurs in the lower abdominal wall due to the following anatomical considerations. Firstly, in the lower abdomen, below the linea semicircularis, only weak transversalis fascia and peritoneum supports the rectus, inferior epigastric vessels posteriorly(1). Secondly, branches of the inferior epigastric pierce the rectus abdominis and are firmly attached to it(1). Thirdly, the rectus is usually crossed by three transverse intersections, with the lowermost segment being the longest; hence, muscle shortening and contraction is the greatest at this level(2).
RSH has been mistaken for many common acute abdominal diseases, such as appendicitis, incarcerated inguinal hernias, urinary obstruction, acute cholecystitis, mesenteric vascular insult, dissecting aneurysms, pregnancy and torsion of ovarian cysts(2). It has also been mistaken for an ovarian tumour(6,7). This is because of the absence of the posterior layer of the rectus sheath below the arcuate line, allowing the haematoma to assume enormous size and hence be palpable on pelvic examination(7).
Diagnosis of RSH can be difficult as evidenced by the high rate of misdiagnosis. A careful history must be obtained to elicit risk factors and precipitating events. Fothergill's sign, an important examination finding, is elicited by having the patient raise his or her head while in a supine position; intra-abdominal masses will become impalpable and abdominal wall masses will become fixed and palpable. A tender mass that does not disappear with contraction of the rectus muscles is indicative of a RSH(4,5).
Imaging techniques like ultrasound and CT scan can be used to help make a diagnosis. Ultrasound in one series of cases was 100% sensitive(1). Failure rates of ultrasound in other series has been reported to be < 30%(2). The ultrasound appearances depend upon whether the lesions extend to any degree below the arcuate line where confusion can occur with other pathology, especially pelvic pathology unless the clinical picture is recognized(6). Above the arcuate line, RSH tend to be limited to ovoid shaped lesions by the anterior and posterior divisions of the sheath. However, beneath the arcuate line, RSH can expand extensively into the extraperitoneal space passing inferiorly, laterally and posteriorly to impinge on the bladder. Initially, the haematoma will present as a trans-sonic cyst-like mass but after fragmentation of the blood some internal echoes will be seen(6).
Three types of RSH can be distinguished by way of the severity of hemorrhage as delineated on CT scans. Type I RSHs are unilateral haematomas contained within the muscles. Type II RSHs are bilateral haematomas or haematomas not contained within the muscle sheath. Type III RSHs invade the prevescicular space or peritoneum(9).
The treatment of RSH comprises rest, analgesia, discontinuation of any anticoagulation therapy, blood and blood product transfusions (if needed) and clinical observation. Surgical procedures may be used for diagnostic purposes as well as in controlling continued hemorrhage or intraperitoneal rupture. In general, surgical procedures consist of clot evacuation, ligation of all bleeding vessels and closed suction drainage(9).
Conclusion
Rectus sheath haematoma is an unusual though not rare cause of a painful abdominal mass that may present to the gynaecologist. A careful history and physical examination and a high degree of suspicion when performing pelvic ultrasound examination will assist in making the correct diagnosis.
Correspondence to
Dr Wee Horng Yen Tel: 63941027 Fax: 62918135 Email: Wee.HY@kkh.com.sg