Unusual Twins: a case of intrauterine pregnancy with complete molar pregnancy
P Kushtagi, T Hegde
Keywords
hydatidiform mole, monozygotic twin placenta, normal fetus
Citation
P Kushtagi, T Hegde. Unusual Twins: a case of intrauterine pregnancy with complete molar pregnancy. The Internet Journal of Gynecology and Obstetrics. 2008 Volume 10 Number 2.
Abstract
A twin pregnancy with one normal fetus and another a vesicular mole is described. The situation presents a significant clinical dilemma. A brief literature review is provided.
Introduction
The cases with gestational trophoblastic disease concurrent with normal intrauterine pregnancy have been reported as being rare as 2.5 to 5 percent of molar pregnancies 1,2 or one in 20,000-1,00,000 pregnancies 3. The clinical entity has aptly been described as Sad Fetus Syndrome 4 and reviewed from time to time.5,6
This presents the physician and patient with significant clinical dilemma between immediate intervention and expectant management, particularly in the case of highly desired pregnancy. The decision will be guided by the problems that may arise and those that are already present. The patient's parity status will also influence the decisions.
Herein reported is one such case of normal intrauterine pregnancy with coexisting complete molar pregnancy.
Case Report
She was aged 22 years. She had regular menstrual cycles of 3-4 days every 28-30 days. She conceived in 4 months of marriage and had first record of pregnancy with positive urine test for hCG at 42 days after the last menstruation. She first reported at 11 weeks 4 days of pregnancy with vaginal bleeding of 15 days duration and lower abdominal pain. Her blood pressure was 140/80 mm Hg and the uterus was palpable in hypogastrium to be of 14 weeks size. Abdominal ultrasound done at that time showed three gestational sacs and only one with fetal pole (Fig.1).
Estimation of beta human chorionic gonadotrophin (hCG) done was 1, 81,759 mIU/mL. Even after 3 weeks of observation on progesterone support with micronised progesterone and folic acid supplementation, vaginal bleeding persisted. At 14 weeks 2 days she noticed and complained of passing ‘grape like vesicles'. The uterus was enlarged to 18-20 weeks size; the blood pressure was 110/70 mm Hg. Repeat ultrasound examination revealed only two gestational sacs, the posterior one with 14 weeks live fetus and the other having vesicular mole (Fig.2). The serum beta hCG was 5, 21,698 mIU/mL.
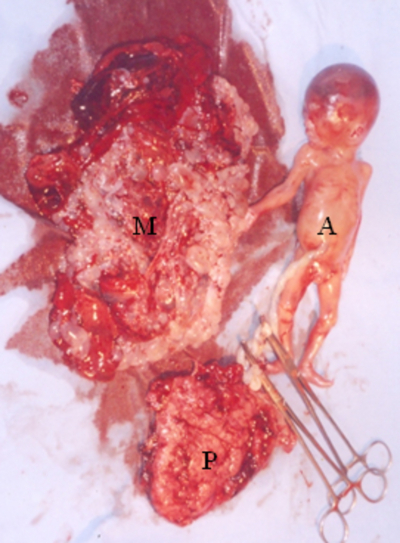
Figure 2
At 16 weeks 2 days, she had spontaneous abortion. First the molar pregnancy was expelled which weighed 500g. It was followed 20 minutes later by a live male fetus with no grossly detectable anomalies, weighing 250g and a placenta of 100g.(Fig.3).Serum beta hCG at this time was 3, 98, 100 mIU/mL and repeat estimate after a week was 3, 10, 500 mIU/mL.
By 4 weeks of abortion the value came down to 321 and was undetectable at 6 weeks post-abortion. The check pelviscan showed uterus of 8.6 x 5.3 cm with anterior wall subserous myoma of 9 x 12 mm and regular, empty endometrial cavity.
Discussion
It was a case of complete hydatidiform mole with coexisting live twin as there were two separate gestational sacs, fetal growth consistent with that for expected age with no obvious anomalies. However, no karyotyping of the conceptuses was undertaken. The high beta hCG value of 1, 81,759 mIU/mL at the very outset or the record of rising value to 5, 21,698 mIU/mL with the widely discrepant higher uterine growth should have prompted immediate evacuation of the pregnancy.
Because most of such pregnancies will be terminated prematurely either because of persisting hemorrhage or severe preeclampsia. Nearly three fourth of the cases do not go beyond 20 weeks of pregnancy.5 The ones that are diagnosed at a more advanced gestational age, having smaller discrepancy between uterine size than that expected by dates, and no or mild preeclampsia are more likely to result in viable surviving infants. Intrauterine death of co-twin or spontaneous pregnancy loss may occur due either to thromboembolic disease or severe preeclampsia. Nevertheless, nearly 40 percent of women who choose to continue their pregnancies have live babies most delivered beyond 32 weeks' gestation.6 Lesser estimates of serum beta hCG and/or those showing decrease early in the second trimester7 may strengthen the decision for expectatnt management. It is also suggested that serially declining serum hCG levels and a documented normal fetal karyotype be considered as requirements for expectant management of these cases to an age fetal viability.8
However, risk of developing persistant gestational trophoblastic tumor (pGTT) should be kept in mind. The determining factor seems to be whether the molar component is partial or complete. Partial moles have a relatively low incidence of 4 percent of producing pGTT when compared to 20 percent risk in complete moles.9 It is not clear whether this increased risk is due to a delay in diagnosis with prolongation of pregnancy or rather an intrinsic propensity toward pGTT. Higher incidence of pGTT was observed for the gestations with complete mole interrupted at a previable stage than those let to progress to a gestational age of fetal viability (68 versus 28%).5 It is hypothesised that even the pregnancies with complete hydatidiform mole and coexistent surviving twin that continue to viable stage suggest benign trophoblast and not to be at any greater risk of developing pGTT solely by virtue of their advanced gestational age.
When a fetus is present in conjunction with partial mole, it generally exhibits the stigmata of triploidy, including growth restriction and multiple congenital malformations.10 This is compatible with both fetal and placental development but not long term survival. While twin pregnancy consisting of a complete hydatidiform mole and coexisting fetus have two separate conceptuses, with a normal fetus and a placenta comprising one twin and a complete molar gestation in the other. Complete moles lack identifiable embryonic or fetal tissues.
Cytogenetically partial moles usually have triploid karyotype with the extra haploid set of chromosomes of paternal derivation. Whereas complete moles have a diploid karyotype that is entirely of paternal origin. 11
Twin molar gestations resulting in a viable live born infant are found to have less discrepantly grown uterus in size, lower frequency of preeclampsia, significantly lower serum beta hCG values and diagnosed later in gestation - all indicating less expansive molar growth or perhaps even molar degeneration and subsequently a more benign clinical course.
The considered absolute indications for terminating pregnancy needs are severe preeclampsia, intractable vaginal bleeding, hyperemesis gravidarum, hyperthyroidism, and evidence of trophoblastic embolisation. In a clinically stable patient an additional relative indication for therapeutic intervention is uterine enlargement markedly greater than that predicted by dates.
It will be difficult to outline the optimal management in gestational trophoblastic disease coexistent with live twin as most of the suggestions are based on either anecdotal case reports or retrospective compilation and analysis of such reports. Whatever the antenatal management approaches for these patients, careful surveillance for the pGTT is warranted. Clinicians should continue to report their experience with these unusual cases as large series of patients will be necessary to formulate a clinical policy.
Correspondence to
Pralhad Kushtagi 1, KMC Quarters MANIPAL 576104 Phone: 91 820 2922592 email: pralhadkushtagi@hotmail.com