The five most common misdiagnoses: a meta-analysis of autopsy and malpractice data
C McDonald, M Hernandez, Y Gofman, S Suchecki, W Schreier
Keywords
diagnosis, malpractice, misdiagnosis, pathology autopsy, quality assessment
Citation
C McDonald, M Hernandez, Y Gofman, S Suchecki, W Schreier. The five most common misdiagnoses: a meta-analysis of autopsy and malpractice data. The Internet Journal of Family Practice. 2008 Volume 7 Number 2.
Abstract
Background
Much research has been done comparing clinical diagnosis with the cause of death determined at autopsy. There have also been many studies that have used malpractice cases to compare initial clinical diagnoses with the final diagnoses. However, there have been no articles that have listed the most common misdiagnoses or complications of the most common combined outcomes of malpractice and autopsy research. Since malpractice claims often involve negligent misdiagnoses, it is important to supplement the autopsy data with the malpractice data. 12 In addition, malpractice cases contain a relatively thorough documentation of the case history and thus can yield valuable information regarding diagnostic breakdowns leading to severe outcomes. 3 Such a list will prove beneficial to physicians, health care personnel, and individuals concerned with quality control and proper practices in the health care setting.
In the United States, there are, on average, 110,000 malpractice claims filed per year, and as many as 98,000 preventable deaths from medical errors. 4 The cost of medical failures is estimated to be between $17 billion and $29 billion. 5 In 2004, a total of $4.2 billion dollars was paid in malpractice lawsuits. 6 The highest payouts (and the most common type of lawsuits) were related to misdiagnosis, failure to diagnose, or delayed diagnosis. These payouts were even higher than other lawsuit causes such as surgical errors. 78 In this paper, the authors present the five most commonly misdiagnosed conditions (as confirmed at autopsy and malpractice proceedings) with the hope of aiding medical personnel and ultimately contributing towards better patient care.
Methods
Data sources
This study focused on studies investigating the association between clinical diagnosis and autopsy and misdiagnosis findings. Searches of PubMed, Embase, and Web of Science databases up to 11 November 2008 using a search strategy that included both truncated free text and exploded MeSH terms. MeSH headings included “misdiagnosis”, “autopsy”, “malpractice”, “diagnosis”, “medical errors”, and their variants was executed. The search strategy had no language restrictions. References were also consulted from the extracted articles and reviews to complete the data bank. When multiple articles for a single study were present, the latest publication was used and supplemented, if necessary, with data from the most complete or updated publication. The relevance of studies was assessed using a hierarchical approach based on title, abstract, and the full manuscript.
Study selection
Studies were identified that evaluated the agreement between clinical misdiagnosis and autopsy/malpractice outcomes. Studies were excluded if they if they did not adjust for potential confounders and/or did not report an adequate statistical analysis.
The initial search yielded 56 reports, of which 23 were excluded on the basis of the abstract. Of the remaining 33 articles, two additional articles were excluded because they represented duplicate studies, thus only the latest or more complete paper was included in the final analysis. Finally, 31 articles fulfilled the inclusion criteria. 1011121314151617181920212223242526272829303132333435363738394041
Data extraction
The following baseline characteristics were extracted from the original reports using a standardized data extraction form, enabling inclusion in the meta-analysis (including lead author, year of publication, country of origin, sample size and number of outcomes and variables that entered into the multivariable model as potential confounders. Four investigators (CM, MH, YG, and SS) collected the data, and disagreements were solved by consensus and by the opinion of a fifth author (WS), if necessary. Outcomes of interest were clinical diagnosis (pre-mortem) and (post-mortem) cause of death according to autopsy and malpractice data review.
The quality of the studies was assessed according to the number of cases and adjustment for potential confounders. Studies with a high number of participants and adjustment for confounders (including demographic, anthropometric, and traditional risk factors were considered to be of high quality.
Statistical analysis
The results of the original studies from multivariable models with the most complete adjustment for potential confounders were used. A random effects model that accounts for inter-study variation and provides a more conservative effect than a fixed model was utilized. A random summary of relative risks was calculated with 95% confidence intervals by using an inverse variance method.
The studies were grouped according to the different clinical outcomes. The potential sources of heterogeneity were assessed using the standard 2 test. In addition, the I 2 statistic was used to investigate heterogeneity by examining the extent of inconsistency across the study results. To examine the potential source of heterogeneity across studies evaluating misdiagnosis, sensitivity analyses were performed according to some characteristics of the studies—country of origin (United States, other countries), pre- and post-mortem diagnosis and the quality of the studies (low, high). Based on this assessment, the most common causes of misdiagnoses were elucidated.
Results
Since it is often difficult to differentiate “misdiagnosis” from “delayed diagnosis,” the term “maldiagnosis” will be used to include both of these categories – that is, not only errors in clinical diagnostic tests or laboratory results, but also mishandling of results and improper follow- up.
The meta-analysis of autopsy data revealed that the five most commonly “maldiagnosed” diseases (based on total incidence) are infections, pulmonary emboli, myocardial infarctions (MI), cardiovascular diseases, and neoplasms (see Table 1).
Further, the five most common maldiagnosed diseases (based on relative incidence) were: pulmonary emboli, myocardial infarction, neoplasms, and cardiovascular diseases.
This ranking is based on the meta-analysis of the results from over 30 different autopsy studies, which analyzed discrepancies between clinical diagnosis and post-mortem autopsy results. 1011121314151617181920212223242526272829303132333435363738394041 The studies analyzed and examined errors in diagnosis in different locations, at various hospitals and among different populations.
We have also included a list based upon the total incidence (Table 2) and one based upon the relative incidence because some diseases, though commonly maldiagnosed, are not more likely to be maldiagnosed than others. For example, the autopsy data shows that infections are the most commonly maldiagnosed diseases (based on sheer number of cases), but because there are millions more infections than the second most commonly maldiagnosed disease (pulmonary emboli), the relative incidence of pulmonary emboli maldiagnosis is actually much higher than that of infections. In fact, when relative incidence is calculated, infections do not make the top five on either the autopsy or malpractice list.
In terms of the
Discussion
The results of this study suggest that patients are much more likely to seek litigation if they are (or were) inflicted with a malignancy than any other disease. This may be because complications related to malignancies are, or are perceived as, more preventable than those related to acute infections, which are the most common maldiagnosis according to the autopsy data. Furthermore, the high rate of pulmonary emboli maldiagnosis may be an important contributor to the large number of deaths from that disease each year. In fact, there are more deaths from pulmonary emboli each year (60,000-200,000) than from AIDS, lung cancer, and motor vehicle accidents combined. 606162
Although it is beyond the scope of this paper, it is worth noting that the most common causes of these maldiagnoses were a diagnostic “blind spot,” such as a conscious decision not to pursue a clinical finding, failure to account for a symptom or sign, atypical presentations and/or inadequate follow-up of abnormal laboratory findings. 63
Moreover, most malpractice cases occurred at physician’s offices and involved primary care physicians. The median interval between the time that clinical symptoms were present and that a patient was diagnosed was 303 days. The most common factors leading to medical errors included failure to obtain a proper medical history, order the appropriate diagnostic tests, or provide adequate follow up. In about 40% of cases, the physician failed to issue a proper follow up plan, perform an adequate physical examination, or interpret a diagnostic test. 3
Since malignancy is an important source of maldiagnosis (12% of cancers are initially misdiagnosed 6465 , and 63% of malpractice cases had to do with a failure in cancer diagnosis 3 ), physicians should pay special attention to proper conduction of diagnositic test, for they are the main reason for diagnostic errors. In fact, the most common reason for filing a malpractice claim against a pathologist was found to be a false-negative diagnosis of melanoma. Moreover, it should also be noted that 57% of malpractice claims included the following five categories: melanoma, breast biopsy, Papanicolaou tests, gynecologic pathology and operational error. 9
In contrast, most of the non-cancer maldiagnoses were due to inadequate history/physical or failure to refer. Indeed, studies have shown that the physician lacked knowledge of the appropriate test or did not think follow up was necessary. Over three quarters of cases were due to failures in judgment, while about half were due to lack of vigilance or memory. Only about one quarter of adverse events were due to negligence itself. 42495366 In a substantial number of cases, there were at least three process breakdowns and at least two clinicians involved. 3
Misdiagnosis of myocardial infarction (MI) becomes more common if the patient does not report symptoms (e.g. not reporting angina) or if the person does not have common risk factors. For example, only 30% of women report chest pain when having a heart attack. Moreover, MI can be confused with a variety of conditions including heartburn, pulmonary embolism, gallstones, bronchitis, gastritis, or nervousness. 67 These findings are especially relevant to emergency physicians, as the top diseases cited in the claims against them included myocardial infarction, aortic aneurysm, infections, hemorrhages, and epiglottitis. 5051
An analysis of the autopsy literature suggested that in about a third of cases the wrong diagnoses was made pre-mortem. However, postmortem analysis suggests that only a minority of these maldiagnosed patients would have benefited from the correct diagnoses being made. 1027 It should also be noted that malpractice claims have a lesser incidence of being filed against physicians who spend more time with their patients (as little as 4 minutes more) and show concern. 4445
Although this study is not meant to be a definitive work on the subject, basic conclusions can be made from its findings. For one, the need for a proper history and physical (as well as rapport and care) is stressed, as well as the need to institute policies, procedures, and systems that reduce the most common process errors that lead to the maldiagnosis of these five most common conditions.
Limitations
Autopsy Data
Potential sources of error and bias were the limitations of those performing the autopsy, abilities of the physicians diagnosing the ailment pre-mortem, regional ‘hot spots’ of diagnoses, sample sizes, facility type, and classification method (among others). Regional ‘hot spots’ are evident as one reviews the literature for papers comparing diagnoses with autopsy-determined causes of death. For example, Sarode, et al 35 found that tuberculosis predominated over the bacterial infections in their study in India in 1993, while others found different illnesses predominated over the bacterial infections in their study. Sample size and facility type are also critical components of the outcome of research (larger and more socially heterogenous studies are more likely a true measure of the activity of the entire population). Lastly, the method by which each institution classified data is a source of bias (e.g. viral and bacterial infections may be lumped together as “infections,” where others may break down the results by individual infection).
The most common maldiagnoses presented are the results of a meta-analysis. Therefore, individual results and levels of misdiagnoses may vary from institution to institution (i.e. not universally applicable).
Malpractice Data
In terms of the malpractice data, retrospective review of records will miss certain breakdowns in the clinical process (such as patient non-adherence), which may have led (or expedited) the adverse outcome, as well as contributing factors (such as fatigue and workload) unless they emerged during litigation. Moreover, a breakdown in one process may have stemmed from a breakdown in another (such as oversights in physical examination could lead to a failure to order the appropriate tests). 3 In addition, the malpractice case reviewers may have had a bias towards finding a particular error due to their knowledge of litigation and compensation outcome. 6869 Further, younger patients injuries and cancer are conditions which may be overrepresented. 4952 Similar to the autopsy aspect of this study, there is a lack of studies that are representative of the national trend in malpractice. Some studies have the essence of random sampling and thus were weighed more heavily.
Exclusion of Psychiatric Disorders
Lastly, due to the complexity of psychiatric disorders and a lack of scrutiny at autopsy, psychiatric data was excluded from both the autopsy and malpractice analysis.
Conclusions and Recommendations
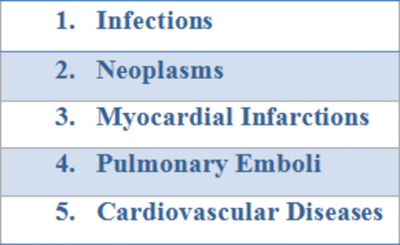
Based upon this research, the five most commonly misdiagnosed diseases, from both an autopsy and malpractice standpoint (based on total incidence) are the following
Figure 5
Moreover, there is a clear need to reduce the rate of uncertainty in diagnosis (since it has been positively correlated to errors 10 ) by employing systems that increase focus on commonly missed signs and symptoms. Since judgment and memory play such a key role in maldiagnosis, systems interventions showing alternative plans and providing clinical decision support should be implemented in a way that fits into a physician’s workflow. 667071 In addition, the system should be automated to detect certain characteristics associated with a particular pathology (especially that which is commonly maldiagnosed). 3
Continuing medical education courses should provide physicians with lists, such as the one compiled in this study, and should educate them as to the critical breakdown points leading to maldiagnosis. Primary care physicians, in particular, would benefit from the information in this manuscript, as they are usually the first physician that the patient presents to. Indeed, targeting the two or three most critical common causes of error may cut the maldiagnosis rate in half.
Acknowledgements