Multivessel Angioplasty
P Upasani
Citation
P Upasani. Multivessel Angioplasty. The Internet Journal of Cardiology. 2002 Volume 2 Number 1.
Abstract
The frequency of multivessel angioplasty is increasing. Multivessel angioplasty is defined as (1) 70% or more diameter stenosis in two or more coronary arteries; (2) 70% or more stenosis in one coronary artery and 50% or more stenosis in a second coronary
artery; or (3) 50% or more stenosis in two or more coronary arteries.1,2,3,4 Quantitative coronary angiography is the most reliable method of assessing severity of a stenosis.
Dilatation In Patients With Multivessel Disease
Multivessel angioplasty involves determination of the complexity of dilatation for each lesion and consideration of other factors such as completeness of revascularization that can be achieved, the results of the procedure, and the impact of restenosis should it occur.
Complete Revascularization
The concept of complete revascularization initially received attention in the surgical literature when outcome was evaluated according to whether patients were completely or incompletely revascularized.5,6 The results of most of these series indicated that patients in whom revascularization was complete had improvement of symptoms and even improved survival (68% to 87% of patients with complete revascularization were asymptomatic compared to only 42% to 52% of patients with incomplete revascularization over a follow-up period of 1 to 5 years). In another surgical series, patients with complete revascularization had improved survival.7 Variables that predicted late survival following coronary artery bypass surgery were the number of diseased but ungrafted arteries, age at operation, and left ventricular function.8
The concept of complete revascularization has been of considerable interest in regard to percutaneous transluminal coronary angioplasty (PTCA) in patients with multivessel disease.4,9,10,11 The ability to achieve complete revascularization depends in part on the definition of complete revascularization which is defined as dilation of all lesions 70% or larger. The ability to achieve complete revascularization depends on the selection of patients. In most series, only about 40% patients with multivessel disease undergoing PTCA had complete revascularisation.2,10,11,12 Hasdai and coworkers13 reported only a slight increase in achievement of complete revascularization that ranged from 50% to 60% over a 16-year period (from 1980 to 1995).
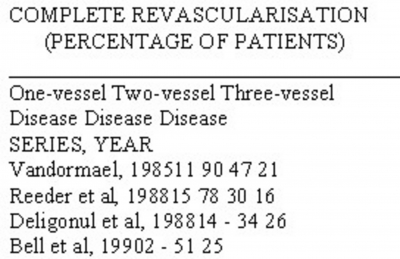
The degree to which complete revascularization is achieved is a function of the extent of coronary artery disease. In patients with single-vessel disease, complete revascularization is achieved in approximately 90% patients with one-lesion dilatation.2,11,14 In patients with more extensive disease, complete revascularization is achieved in approximately 50% of patients with two-vessel disease and 20% to 30% of patients with three-vessel disease (Table 1).
Figure 1
The most common reason for failure to achieve complete revascularization is the presence of a chronic total occlusion.14 In the NHLBI PTCA Registry,16 the commonest reason for incomplete revascularization was that, although the lesions were amenable to PTCA, the operator did not intend to dilate them. The strategy of dilating only those lesions believe to be principally responsible for a patient's ischaemia has been termed as culprit lesion strategy. The second commonest reason for incomplete revascularization was that not all lesions were amenable to PTCA, usually as the result of a chronic total occlusion. Event-free survival is improved in patients with complete revascularization in that the incidences of death, myocardial infarction, and recurrent angina are decreased. 10,11,15
An additional complicating factor is restenosis. The more lesions that are dilated, the higher the restenosis rate per patient. This increased restenosis rate may negate the positive features of being able to achieve complete revascularization. Patients with persistent complete revascularization (i.e. with no restenosis) are likely to have better
outcomes compared to patients with transient complete revascularization (with restenosis).
Differences in outcome may depend on the definition of complete revascularization and assessment of myocardial viability. If the myocardium shows no evidence of regional wall motion, it may not be necessary to dilate the vessel and revascularize the region. Therefore, although complete revascularization may be associated with improved
outcome, it may not always be necessary. This concept has particular importance in patients with multivessel disease.
Target or culprit lesion can be identified by clinical and historical data, electrocardiographic findings, angiography supplemented by radionuclide studies,
intravascular ultrasonography or Doppler wire etc. Morphological characteristics that are associated with an unstable or culprit lesion include scalloped edges, irregular borders and the presence of intraluminal filling defects.
Functionally adequate revascularization, which has received considerable attention, is defined as successful dilation of all stenoses that are 70% or greater in vessels more than 1.5 mm in diameter that supply viable myocardium with residual contractile function.18 Thus, revascularization can be incomplete (not dilating an occluded artery proximal to an infarcted territory or a tiny branch vessel) but adequate.
Initial Results and Follow-up stents have the potential to dramatically change the follow-up of patients treated for coronary artery disease. Questions raised about the durability of stents have been settled by longer-term angiographic studies.19,20
There is limited long-term follow-up of multivessel-stented patients. More data is available on the long-term outcome in patients with multivessel disease treated with balloon angioplasty though results are variable. Different definitions of success have been used: an angiographic success rate per lesion or per patient, and a clinical success rate. Using one of these two definitions of success, high primary success rates have been reported ranging from 85% to 95%.2,14,21,22
Analysis of events during follow-up is problematic. Results from several studies 4,14,23 indicate that most patients are improved following successful PTCA, and the incidence of death (1% to 5%) and nonfatal infarction (approximately 2% to 3%) is low during intermediate-term follow-up. Only approximately 60% of patients remain asymptomatic for a prolonged period. Stents are associated with decreased need for subsequent procedures. Factors independently predictive of combined adverse cardiac events of death, infarction, or coronary artery bypass graft (CABG) surgery were advanced age, presence of rest angina at the time of initial dilation, diabetes mellitus, left anterior descending stenosis location, and left ventricular dysfunction.3 A corollary which arises is that patients with more severe angina, those with more extensive coronary artery disease with a larger ischaemic burden, and particularly those with left ventricular dysfunction may be the ones in whom complete revascularization is most important for achieving not only high survival rates, but also high event-free survival rates.
The need for repeat procedures, either repeat dilation or CABG, during follow-up has varied in the reported series. In patients in whom PTCA was initially successful in reducing symptoms but in whom angina returns during follow-up, repeat PTCA or stenting is most commonly performed. For patients in whom PTCA never satisfactorily improved symptoms, CABG may be more appropriate.
Mabin and colleagues10 and Vandormael and colleagues11 found that event-free survival was significantly better in patients who had complete revascularization than in those who had incomplete revascularization. In the PTCA registry, the adjusted estimates of death and myocardial infarctions, or angina did not differ among patients with complete and those with incomplete revascularization; the latter group, however, had a higher incidence of subsequent CABG during follow-up.15 Similar results were obtained from the data reported by Deligonul and coworkers.14 Follow-up results after multivessel angioplasty are affected by undilated vessels, restenosis, and disease progression, the last one accounting for recurrent symptoms in 9% to 11% of patients.24
Given that complete revascularization is achieved in only one-third to one-half of patients with multivessel disease undergoing PTCA, follow-up of patients with incomplete revascularization is of great importance. In patients undergoing multivessel angioplasty no significant difference as regards overall survival and follow-up angina is observed between complete and incomplete revascularization groups. Perhaps the strongest evidence that complete revascularization is not critical can be found in the randomized trial comparing PTCA and CABG in patients with similar disease.25
Considerable interest has been directed at identifying the culprit lesion in patients with multivessel disease. In those patients in whom a culprit lesion or lesions can be determined reliably with electrocardiography, radionuclide, clinical, or angiographic findings singly or in combination, it appears to significantly improve the long-term results of multivessel PTCA. When the culprit lesion (or lesions) are reliably identified, dilation can be used to treat that lesion alone without exposing the patient to the risks of dilating other lesions not principally responsible for the patient's symptoms. However, it is too early to determine what role dilation of just the culprit lesion should play. Given the information from natural history studies on the importance of the number of diseased vessels, longer-term follow-up studies are needed. Patients with the greatest ischaemic burden may require the most complete revascularization to achieve good long-term event-free survival.
At one-year follow-up, using a composite outcome of death, infarction, or coronary artery bypass surgery, patients with functionally adequate revascularization did nearly as well as patients with complete revascularization and did substantially better than patients with functionally inadequate revascularization. 18
Risks
The risk-benefit ratio must be assessed carefully for each patient with multivessel disease. The risks of complications with PTCA depend on several factors, including specific anatomic features of the artery and lesion to be dilated, the overall cardiac and
noncardiac condition of the patient, and the clinical setting in which dilation is planned. Stent implantation has markedly decreased the incidence of acute or threatened closure and need for emergency CABG.
In the initial PTCA Registry,26 risk factors for acute closure were severity and eccentricity of the lesion, nondiscrete lesions, female gender, unstable angina, and right coronary artery location. Additional risk factors identified by Ellis and colleagues27 include multivessel coronary artery disease, lesion eccentricity, a calcified lesion, a long lesion, female gender, and intimal dissection; the last risk factor resulted in a 6.5-fold increase in the risk of emergency CABG, myocardial infarction, or death. Angiographic risk factors of acute closure are lesion length, female gender, lesion angulation, branch point stenoses, presence of intracoronary thrombus, multivessel disease, and diffuse stenoses in the same vessel. Other investigators have also found thrombus to be associated with a major increase in the incidence of acute closure.24
Presently although more complex lesions and sicker patients are being taken for multivessel angioplasty, the success rates have increased and complication rates have remained the same or improved.13 Studies associating clinical and angiographic characteristics and clinical outcome all will need to be repeated in the current era of widespread stent implantation using high-pressure inflation and newer antiplatelet drugs such as ticlopidine, clopidogrel and glycoprotein IIb/IIIa receptor blockade therapy.
Restenosis
Restenosis remains the Achilles heel of PTCA. Medical strategies aimed at preventing restenosis have expanded greatly and have been tested now in well-controlled, randomized studies. As yet, however, none of these medical approaches has been shown to convincingly reduce the problem, although recently in a single study, abciximab has been shown to decrease clinical restenosis.28 New interventional approaches with excimer laser, directional atherectomy, rotational atherectomy, and stents have been evaluated. The best data suggesting a device-related reduction in restenosis are with stents with a dramatic reduction of short-term complications and restenosis in selected patients.
Following multilesion or multivessel dilation, the risk of restenosis for each lesion does not appear to be completely independent of the other lesions dilated.3,29 Accordingly, the frequency of restenosis for patients undergoing multilesion angioplasty is less than if the risk of restenosis for each dilation site was additive. It is true, however, that the risk of restenosis in a patient increases with each additional lesion that is dilated. Nobuyoshi and coworkers 30 found that patients with multivessel disease and complete revascularization had significantly higher restenosis rates per patient (74.2%15.4%) than patients with multivessel disease and incomplete revascularization (53.8%11.7%). Deligonul and colleagues14 found that the incidence of multilesion restenosis was significantly greater in patients with three-vessel disease than in those with two-vessel disease. The effect of lesion morphology on restenosis is unclear. Patients with rest pain generally have unstable lesions with thrombus present and a higher restenosis rate. Intravascular ultrasonography is currently being evaluated to determine if specific patterns of arterial response to dilation can be used to predict subsequent restenosis. Stent implantation has been definitely shown to decrease angiographic and clinical restenosis rates in selected patients and lesion groups. However, when in-stent restenosis occurs it has major implications.31,32 Recently introduced drug eluting stents have been shown to significantly reduce restenosis after coronary angioplasty with stent implantation.33
Recommendations And The Future
The role of dilation in multivessel disease has been carefully evaluated by several randomized trials of PTCA versus CABG. These trials convincingly document
that the hard end points of death and Q wave myocardial infarction were not different between these two modalities. Both advances in percutaneous techniques (best demonstrated by stents including drug eluting stents) and surgical advances (the less invasive MIDCAB) to a lesser extent have changed the face of revascularization therapy. In addition these trials did not use glycoprotein IIb/IIIa receptor blockade drugs that improve both early and perhaps longer-term outcomes. The future role of interventional cardiology depends on continued technologic advances that are likely to include the use of covered and drug eluting stents, radiation to prevent or effectively treat restenosis, better methods to assess the outcome of PTCA to determine if stent placement is required to optimize the result, and improvements in our ability to treat chronic total occlusion. What is the role of dilation in patients with multivessel disease? The answer depends on the skill and experience of the operator, the patient's anatomy, the clinical condition, the preferred method of revascularization, the setting in which the revascularization is planned, and the patient's expectations. For each patient, the risk-benefit ratio should be examined and discussed with the patient and family. The procedure should be performed only after considering all the options and possible outcomes, preparing for adverse outcomes, and reviewing all these issues with the patient, relatives, and the referring physician.