Spontaneous Haemothorax: Report Of Two Unique Cases Admitted To The Surgical Critical Care Unit
A Channa, A Hussain
Keywords
and warfarin, primitive neuroectodermal tumor, spontaneous hemothorax
Citation
A Channa, A Hussain. Spontaneous Haemothorax: Report Of Two Unique Cases Admitted To The Surgical Critical Care Unit. The Internet Journal of Anesthesiology. 2004 Volume 9 Number 2.
Abstract
Hemothorax is a well-recognized sequel of chest trauma, ruptured aortic aneurysm, inadvertent vessel damage during central veins cannulation, intercostal tubes, pulmonary infarct, intrapulmonary arteriovenous fistula, neoplasm etc. We report two cases of spontaneous hemothoraces which were admitted in our Surgical Critical Care Unit. The first case, a Peripheral Primitive Neuroectodermal Tumor (p PNET) has never been reported and the second case is related to a Warfarin overdose, the second to be reported in the literature.
Introduction
We would like to report two cases of spontaneous hemothoraces, one occurring in Peripheral Primitive Neuroectodermal Tumors and the second after a dynamic hip screw for fracture of neck of femur. Peripheral Primitive Neuroectodermal Tumors (p PNET) are a group of highly cellular primitive round cell neoplasms which occur extra-cranially in soft tissue and bones and are derived from the embryonal neural crest cells. They may arise from the chest wall, skin, orbit, kidney, etc. and tend to be locally invasive or metastasize to distant tissues of the body [1]. Bleeding is a well-established potential complication of anti-coagulation therapy.
Case Reports
Case 1
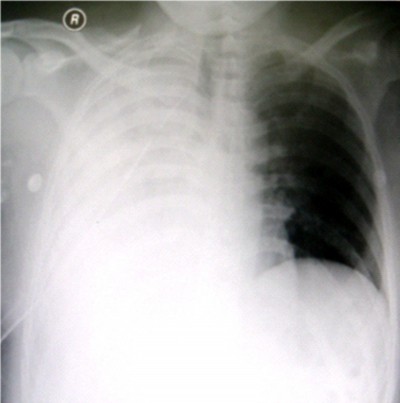
A 35 year old male patient was admitted in our hospital with multiple swellings on the left forearm with distal ischemia of the limb. Conservative management failed to cure the disease. He refused to undergo above elbow amputation as a last option. He was then admitted to another hospital where his left arm was amputated above the elbow. Histopathology report showed a Peripheral Primitive Neuroectodermal Tumor. After one month of amputation, he again came to the Accident and Emergency department of our hospital with a history of bleeding from the amputated stump for the last three days. On his admission he looked pale, the pulse rate was 140/minutes and B.P 120/65 mm of Hg. Air entry on the right side of chest was decreased. Haemoglobin was 6.8 g/dl. Coagulation profile and Liver Function Tests were normal. X-ray chest showed white right lung field as shown in figure1.
Figure 1
He received two units of pack red blood cells. The intercostal tube was inserted and it drained 4 liters of frank blood in the first few hours. He was taken to the Angio Unit for embolization of the left distal brachial artery. Multiple small feeders were coiled up second time as shown in figure 2.
Figure 2
Pulmonary Artery angiography was done in the same session and was normal with no definite source of bleeding. After embolization, the stump continued to bleed minimally and the chest tube drained blood 70-100 ml/hour. Haemotherapy with Packed Red Blood Cells, Platelets, Fresh Frozen Plasma and tranexamic acid continued but all in vain. He then underwent right thoracotomy. Multiple ulcers were found on the surface of the right lung. Biopsies were taken and oozing points were cauterized. The patient was brought to the Surgical Intensive Care sedated, intubated and ventilated. He remained in the SICU for a couple of days and was then discharged to the surgical floor with no bleeding from the stump and pleural space. A histopathology report turned to be metastatic lesions of the same nature as that of the primary tumor.
Case 2
A 90 year old female with long standing diabetes, hypertension, Alzheimer disease, cholelithiasis and osteoarthritis presented to our hospital. She had a history of pulmonary embolism three years back for which she was on warfarin 1 mg daily. She had also history of open reduction internal fixation with a dynamic hip screw (DHS) 3 months back.
Upon her admission Prothrombin Time +INR was 1.13, total Bilirubin 13 umol/L (3-17) and Alanine Aminotransferase 31U/L (20-63). A X-ray chest was normal. Warfarin was held on for surgery. She underwent open reduction and internal fixation for right fracture of the neck of the femur with DHS under general anesthesia. The intraoperative course was uneventful. The trachea was extubated on the operating table and she was then brought to the surgical ICU for observation. She remained in the SICU for three days and then was discharged to the surgical ward. During her stay in the SICU she did not receive any anticoagulant therapy.
Anticoagulant therapy was resumed on the ward after consultation with the hematologist to keep PT+INR 2-3 times of normal:
After 8 days of discharge from the SICU she became restless, agitated and haemodynamically unstable. There was decreased air entry on the right side of the chest. A chest X-ray revealed a totally white right lung field. The patient was intubated electively at this stage. Spiral CT Scan of the chest ruled out the possibility of pulmonary embolism and confirmed the chest x-ray findings i.e., haemothorax/pleural effusion as shown in the figure 3.
Figure 4
She was then admitted to the Surgical ICU. On her admission, the pulse rate was 115/minute, BP 75/40 mm of Hg and Haemoglobin 5.5 g/dl. Two units of Packed Red Blood Cells, 3 units of Fresh Frozen Plasma and an Injection of Vitamin K 1 mg intravenous stat were given. Fiberoptic bronchoscopy showed hyperemic and edematous mucosa. There were no secretions or bleeding in/from the tracheobronchial tree respectively. The intercostal tube was inserted in the 6th right intercostal space and it drained 1500 ml of blood immediately.
Discussion
Primitive Neuroectodermal Tumors (PNET) are malignant small cell neoplasms mainly occurring in children but can occur at any age [2] Peripheral Primitive Neuroectodermal Tumors (p PNET) usually arise either from bone or soft tissue including chest wall, near the spine, pelvis, arms or legs. They belong to the Ewing Sarcoma family of tumors. The symptomatology of the Peripheral Primitive Neuroectodermal Tumors is related to the size and their location. In our case, the tumor was primarily originating from the forearm causing ischemic changes and later on metastasized to the right lung causing a spontaneous haemothorax. This is the first case of Peripheral Primitive Neuroectodermal Tumor causing a spontaneous haemothorax to be reported but the mechanism seems to be very simple, that is, invasion of blood vessels of the lung tissue by the secondries.
Bleeding complications are well recognized when anticoagulant drugs are used. Robinson et al [3] reported a case of spontaneous hemothorax 20- hours after percutaneous transluminal coronary angioplasty (PTCA) in a 74 year old lady with the use of heparin. Similarly, Nasilowski J and Krenkle R [4] reported spontaneous hemothorax in a 76 year old male patient who was on warfarin therapy. His INR was 15.5 and in our case it was 5.23. We agree with the authors that some toxic or allergic reactions are the possible culprits causing spontaneous hemothorax.
Acknowlwdgements
We are thankful to Mr. Sagheer Ahmad, secretary Surgical Intensive Care Unit for providing us medical record related to these two patients.
Correspondence to
Dr.Altaf Hussain, MBBS; DA; MCPS; FCPS. Specialist Department Of Anesthesiology And Critical Care (41) King Khalid University Hospital Post Box No.7805 Riyadh 11472 Saudi Arabia Fax No.: 0966-1-4679364 Phone No.: 0966-1-4671597 E-Mail: Altafdoa@Hotmail.Com