Delayed Traumatic Hernia Of Diaphragm And Pericardium Causing Deterioration During Weaning From The Mechanical Ventilation.
S Kinthala, M Fakoory, A Smith, T Semei, K Johnny
Keywords
cardiac tamponade, diaphrgam, mechanical ventilation, weaning
Citation
S Kinthala, M Fakoory, A Smith, T Semei, K Johnny. Delayed Traumatic Hernia Of Diaphragm And Pericardium Causing Deterioration During Weaning From The Mechanical Ventilation.. The Internet Journal of Anesthesiology. 2012 Volume 30 Number 4.
Abstract
Diaphragmatic injuries are relatively rare and result from either blunt or penetrating trauma. Intrapericardial diaphragmatic hernia (IPDH) hernia is a rare complication of diaphragmatic rupture, occurring in less than 1% of cases of diaphragmatic hernias (DH). IPDH presentation can range from being asymptomatic to having potentially fatal cardiac tamponade. This is a case of delayed traumatic hernia of diaphrgam and pericardium that resulted in deterioration during weaning from the mechanical ventilation. The patient underwent surgical repair for diaphragmatic hernia and reduction of pericardial contents through thoracic approach following which the patient was weaned successfully from the mechanical ventilation.
Introduction
Acquired diaphragmatic hernia can occur as a result of blunt or penetrating trauma. The diagnosis requires a high index of suspicion. Delay in detecting and repairing diaphragmatic injury increases both morbidity and mortality1. IPDH is very rare, occurring in less than 1% of cases DH 2 .Cardiac tamponade is present only in 7% to 10% of IPDH2, 3. We report a case of delayed traumatic hernia of the diaphragm and pericardium that was diagnosed at six weeks after initial trauma. The patient deteriorated during weaning from the mechanical ventilation which was associated with hemodynamic disturbance. The further work up led to diagnosis of IPDH. The patient was managed successfully in our surgical intensive care unit (SICU).
Case description
A 65 year old obese female with no known chronic illness was involved in a motor vehicle accident and sustained multiple injuries. She presented with a Glasgow Coma Scale (GCS) of 3/15 and was intubated. Trauma series workup showed right frontoperital cerebral contusion and left intracerebral bleed in the frontoperietal region. She also sustained fracture of right 1 st, 2 nd; left 6 th and 7 th ribs anteriorly; unstable bipedicular fracture of thoracic vertebra (T) 6 and bilateral laminae T 7 with anterior subluxation of T 7 – T 12 as a unit. Abdominal computerized tomography scan (CT) was normal. Patient was admitted to the SICU for further management.
On day 2 of admission sedation break was given and neurologic assessment showed GCS of 3T/11; on day ten patient underwent tracheostomy in view of anticipated prolonged ventilation. Thoracic spine fixation was considered for stabilization but, as the patient was septic with temperature (temp) 390 C, White cell count 20 K/µL and blood culture positive for pseudomonas aeruginosa, a thoracic brace was placed instead. In the next two week attempts to wean from mechanical ventilation were unsuccessful due to severe sepsis and traumatic brain injury. Neurologic assessment at week 3 of admission showed that the patient had spontaneous eye opening with GCS 7 T/11. At week 5 of admission, after resolution of sepsis patient underwent thoracic spine stabilization and dorsal fusion with pedicle screw fixation at T 4, 5 7, 8 for unstable bipedicular fracture of T 6. Both surgery and anaesthesia were uneventful.
In the 6 th week (day 37-40) following the fixation of thoracic spine surgery patient was weaned from synchronised intermittent mandatory ventilation (SIMV) settings of Tidal volume (TV) 500 ml, Respiratory rate (RR) 12 breaths/min, Pressure support (PS) 14 mmHg, Positive end expiratory pressure (PEEP) 6 mmHg, Fio2 40% to continuous positive airway pressure (CPAP). Patient was generating TV of 500 ml. Arterial blood gas analysis (ABG) on CPAP with PS of 12 mmHg and PEEP 6 mmHg and Fio2 40% was pH 7.5, Pco2 33 mmHg, Po2 142 mmHg, Hco3 28 mmol/L, Base excess +4mmol/L. Patient was tolerating T- piece trials for approximately two hours, weaning was continued and neurological status improved with GCS 7 T/11.Vitals were heart rate (HR) 91 beats/min, Blood pressure (BP) 132/71 mmHg, T 370 C, Respiratory rate (RR) 18 breaths/min.
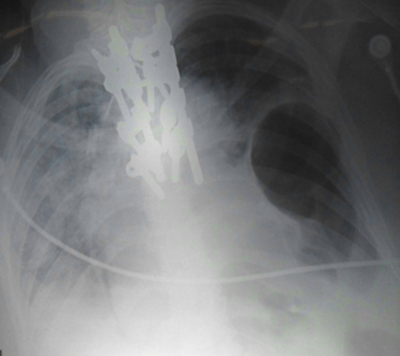
Over the following two days (day 41- 42) the patient was continued on T - piece trials during which she deteriorated and became increasingly tachypneic, hypotensive and tachycardic, eventually requiring SIMV for respiratory support. The patient’s urine output declined and was unresponsive to volume resuscitation. During this period the central venous pressure rose from 6 mmHg to 14 mmHg. She also required increasing doses of noradrenaline for blood pressure maintenance. Vitals were HR 121 beats/min, Temp 370 C, BP 127/60 mmHg. The ABG on SIMV with settings of TV 500 ml, RR 12 breaths/min, PEEP 8 mmHg, PS 12 mmHg, Fio2 40%, showed pH 7.3, Pco2 35 mmHg, Po2 122 mmHg, Hco3 20 mmol/L, Base excess -5 mmol/L. The differentials considered for the deterioration during weaning were sepsis, anaemia, acute coronary event, pulmonary embolism, lung collapse, low GCS, nutritional issues and delayed diaphragmatic hernia. Full blood count, biochemical profile and cardiac enzymes were within normal limits. On clinical examination decreased air entry was noted in the left base of the lung. A 12 lead ECG showed sinus tachycardia, transthoracic 2D echocardiography was attempted but unsuccessful due to poor acoustic window. A chest x ray revealed left lung base opacification and bowel loops in the chest (Figure: 1) which were not present on the previous chest X ray. A diagnosis of diaphragmatic hernia was made. Patient was prepared for the surgical repair of diaphragmatic hernia.
Figure 1
The patient received general anaesthesia and induction was without significant hemodynamic instability. Single lung ventilation was instituted with placement of left bronchial blocker for left lateral thoracotomy. At thoracotomy loops of transverse colon and accompanying omentum were protruding through defect in the pericardium in to the left pleural cavity (Figure: 2 and 3). The colon had entered the pericardium through 8 cm defect in the central tendon of diaphragm. The pericardium was incised anterior to phrenic nerve to expose bowel contents and the diaphragmatic defect. After the reduction of the bowel into the abdomen, the diaphragmatic defect was closed with Gortex patch and pericardium was left open.
Figure 2
Figure 3
Intraoperatively there were no complications. Following surgery patient was hemodynamically stable and noradrenalin was discontinued. The Patient was transferred to SICU for elective mechanical ventilation. The post operative chest x ray and transthoracic 2 D Echo were unremarkable.
In the following week patient was successfully weaned from SIMV on setting TV 500 ml, RR 12 breaths/min, PS 12 mmHg, PEEP 6 mmHg, Fio2 40% to CPAP with PS 12 mmHg and PEEP 6 mmHg and Fio2 40%, then to T piece on Fio2 40%. (ABG on T piece was pH 7.35, Pco2 38 mmHg, Po2 112 mmHg, Hco3 22 mmol/L, Base excess - 4mmol/L) later to spontaneous breathing .The tracheostomy was decanulated and she was subsequently shifted to the ward with normal vitals and labs, with GCS 11/15.The patient was discharged after two months of rehabilitation therapy, with GCS 15/15 .
Discussion
Diaphragmatic injuries are relatively rare. Incidence of blunt diaphragmatic rupture (BDR) is 1.9%. Among those with BDR, 65 % have a tear on the left side of the diaphragm, 22.5% have a tear on the right side and 2% have a tear on both sides4. Road traffic collisions are the most frequent causes of diaphragmatic rupture5. Delayed traumatic diaphragmatic hernias are defined as those, which present at one month or more after trauma. Up to 30% diaphragmatic hernias present late6. Delay in presentation of a diaphragmatic hernia could be explained by the fact that delayed detection of a diaphragmatic defect which occurred with injury manifesting only when herniation occurs7. Extubation precipitates this phenomenon when the intrathoracic pressure becomes negative7. When diaphragm ruptures, this pressure difference causes the abdominal viscera to herniate through the defect into the chest cavity.
IPDH is a sacless hernia directly through a rent in the pericardial portion of the diaphragm. The organ most frequently involved in traumatic IPDH appears to be the transverse colon, followed by the stomach and the greater omentum .The IPDH most frequent clinical symptoms are respiratory (40% of cases) and gastrointestinal (38% of cases) 3. Physical findings of IPDH include bowel sounds in the chest, decreased heart and lung sounds and an absent point of maximal cardiac impulse. Associated injuries are frequent, and there is a predominance of rib fractures and head injury3.
Our patient had cardiorespiratory signs but no gastrointestinal signs. Individuals with IPDH tend to show features of cardiac compression. Herniation of visceral contents into the pericardial sac reduces ventricular filling, stroke volume, and thus decreases cardiac output. Cardiac tamponade is an immediate sign in the large posttraumatic defect of the pericardium3.
The high pressure ventilation of the endotracheal anaesthesia causes further reduction in venous return and cardiac output, exaggerating the effect of IPDH, and sometimes precipitating cardiac arrest. If cardiac arrest occurs external cardiac massage may provide temporary improvement but urgent thoracotomy may be needed for the definitive management. Our patient was on mechanical ventilation receiving sedation with midazolam and fentanyl preoperatively .We continued the inotropic support and induced the case with ketamine and fentanyl to avoid any hemodynamic deterioration at induction.
The diagnosis of traumatic IPDH is considered on the basis of a chest x-ray and clinical features. Additional diagnostic tools are CT scan, contrast studies, and echocardiography. In our patient transthorasic echocardigraphy was not successful due to poor acoustic window which was probably due to the bowel contents in the pericardium .CT scan was deferred to avoid any events during the transportation, as the patient was on mechanical ventilation and requiring high doses of vasopressors to maintain adequate blood pressure.
In the absence of a hernia, it may be difficult to identify traumatic diaphragmatic injury on conventional imaging and many patients with diaphragmatic hernia require mechanical ventilation; however, paradoxically, once mechanical ventilation is started, detecting a diaphragmatic injury on radiographs may become more difficult because the positive pressure ventilation may push herniated contents down8. The initial chest radiograph can be negative and a repeat chest radiograph may be necessary for diagnosis9.
In this case, while the patient was on SIMV and respiration was fully supported there were no symptoms of respiratory embarrassment. The weaning was successful initially but deteriorated as weaning progressed, possibly due to the negative intrathoracic pressure created during spontaneous respiratory efforts of weaning leading to the herniation of the intra abdominal contents through diaphragmatic defect. In accordance to the pressure gradient between the abdominal and thoracic cavities the contents of IPDH increased progressively causing a pressure effect on the heart and myocardial dysfunction leading to hemodynamic disturbance resulting in tachycardia, and necessitating noradrenalin for blood pressure maintenance. In this case hemodynamic disturbance due to IPDH resulted in deterioration of patient during weaning.
The thoracic approach is used for the surgical management in 64% of the IPDH diagnosed in the delayed phase. The thoracic approach is preferred as adhesions in the pericardium can be freed more easily3. In our case the preoperative diagnosis was of a diaphragmatic hernia, but to our surprise the herniated bowel contents were entering in to the pericardium through a diaphragmatic defect and then into the left hemithorax through a separate pericardial defect. In retrospect we hypothesise that omentum and transverse colon entering in the pericardium through central tendon defect might have caused myocardial dysfunction due to increased intrapericardial pressure, but still did not lead to acute cardiac tamponade. This may be due to the fact that contents were able to exit through the pericardial defect in to the left pleural cavity, relieving intrapericardial pressure. Post operatively once the contents of the pericardium were reduced and diaphragmatic hernia was repaired. The patient hemodyanmics improved remarkably maintaining normal blood pressure without noradrenalin. Post operatively weaning was successful due to improved pulmonary and cardiac function.
In Conclusion, blunt diaphragmatic rupture resulting in IPDH is rare. Therefore it is wise to have high index of suspicion for diaphragmatic injury in those patients who are victims of vehicle collisions. Delayed IPDH needs to be considered as one of the possible differential when a patient deteriorates during the process of weaning from mechanical ventilation.