A Prospective Randomised Study Of Combination Of Epidural Bupivacaine With Clonidine And Bupivacaine For Postoperative Analgesia
Jyothi, H Verma, S Safiya
Citation
Jyothi, H Verma, S Safiya. A Prospective Randomised Study Of Combination Of Epidural Bupivacaine With Clonidine And Bupivacaine For Postoperative Analgesia. The Internet Journal of Anesthesiology. 2012 Volume 30 Number 2.
Abstract
Introduction
Epidural analgesia is the most common and most widely used neuraxial technique for providing safe, reliable postoperative analgesia. The earliest agent used was epinephrine. Epidural ketamine went out of favour as inadvertent intrathecal use was associated with neurotoxic effects. Epidural neostigmine was used and had high incidence of nausea and vomiting1.
Currently epidural opioids are an established and accepted technique. Epidural opioids provide excellent, prolonged and segmental analgesia without causing autonomic or motor blockade but are associated with undesirable side effects like respiratory depression, pruritis, sedation, nausea, vomiting2.
Clonidine is a selective partial alpha-2 adrenergic agonist with a selectivity ratio of 200:1 in favor of alpha-2 receptors. US FDA-approved preservative-free clonidine formulation meant for epidural use in 1996. In recent times, the role of epidural clonidine for relief of postoperative pain promises a new platform in this field3.
The current prospective randomized double-blind study was undertaken in surgical patients to evaluate the comparative hemodynamic, analgesic, sedative and respiratory effects of clonidine in patients receiving epidural analgesia.
Methodology
After obtaining institutional ethical committee approval and written informed consent, 90 adult patients, ages 30-75 yrs, of either gender belonging to ASA physical status 1 and 2 scheduled for abdominal, obstetrical, gynecological and orthopedic surgery under epidural anaesthesia, during the study period (Jan 2009 - Dec 2009) were recruited.
Patients for whom central neuraxial block was contraindicated and those with history of poorly controlled hypertension, angina, congestive cardiac failure, atrial fibrillation, arrhythmias, weight >95kg, age >75years, ASA grade 3 and 4, on tricyclic anti-depressants, alpha-2 adrenergic agonists or opioids were excluded from this study.
On the day prior to the surgery, a detailed medical history was taken and systemic examinations were carried out. Necessary laboratory investigations were done. Patients were explained about Visual Analogue Scale (VAS) and were taught how to express the degree of pain on the scale.
Randomization was done by using computer-derived random number sequence and sealed opaque envelopes and all investigators were kept unaware of the envelope details throughout the whole study period. After intravenous (IV) access, an infusion of ringer’s lactate (20ml/kg) comprised preloading. All patients had an epidural anaesthetic with 18 G Tuohy needle. The epidural space was identified at L2-3 or L4-5 using loss of resistance technique under strict asepsis and a 20 G epidural catheter was then advanced for 3-5cm into epidural space. Correct placement was verified with a test dose of 3ml epidural lignocaine with 1:2,00,000 adrenaline. Surgical procedure carried under 0.5% bupivacaine in intermittent bolus doses.
At the end of surgery patients were shifted to recovery room. When the patient first complained of pain, they were shown VAS and were asked to express the intensity of pain on the scale. When it reached >4 mark on the scale, they were allocated to receive either
B: Plain bupivacaine 0.125% 10ml. (n = 35).
BC: clonidine 150ug (1ml) + 0.125% bupivacaine 9ml.(n = 35).
Monitoring consisted of pulse rate, respiratory rate, non-invasive blood pressure (Systolic blood pressure (SBP)/ diastolic blood pressure (DBP) measured preoperatively, intraoperatively and postoperatively. Incidence of bradycardia (pulse rate<60/min), hypotension (fall in SBP> 30% of baseline and fall in DBP > 15% of baseline), nausea, vomiting, urinary retention, pruritis, shivering were noted.
Duration of analgesia, that is the time of onset of sensory block of dose until request of 1 st analgesia, was noted. Rescue analgesia with intramuscular diclofenac was given and study stopped.
Postoperatively SBP/DBP, respiratory rate and pulse rate were measured every 15min in 1sthr and at 1.5,2,3,3.5,4,5,6,8,12,24 hrs or until the time when pain reappeared.
Sedation score every 15 min in 1 st hr and 1.5,2,3,3.5,4,5,6,8,12,24 hrs or until the time when pain reappeared.
Visual Analog Score every 15 min interval for 1 hr and 1.5,2,3,3.5,4,5,6,8,12,24 hrs. Visual Analogue Scale (VAS) was used to assess the intensity of pain and pain relief. This scale consisted of a 10 cms line, marked at 1cm each, on which patient expresses the degree of pain by placing a point. Mark “0” represents no pain and mark “10” represents worst possible pain. At the time at which rescue analgesia was given, the patient was asked to give a global assessment of the overall effectiveness of the analgesic treatment.
Quality of analgesia (table 1) was assessed and compared in both the groups.
Adverse effects like hypotension (fall in systolic blood pressure by >30% or fall in diastolic blood pressure by 15%), bradycardia (pulse rate <60/min), respiratory depression (RR<10/min), sedation, shivering, dry mouth, nausea, vomiting, drowsiness, urinary retention and pruritus were noted in postoperative period.
The statistical analysis of data was done using -
Observation And Results
The mean age (table-2) in both the groups is comparable (50.77 yrs in group B and 50.51 yrs in group B+C). The maximum and minimum age in group B were 70 yrs and 32 yrs and in group B+C were 71 yrs and 29 yrs. The ASA status and the sex incidence in both groups B and B+C are also similar.
TABLE 3 : ANTHROPOMETRIC COMPARISON
The mean weight (table 3) in group B and B+C are comparable (46.7 kg and 47.9kg). The maximum and minimum weights in group B were 58 kg and 42 kg and in group B+C were 56 kg and 41 kg. The mean height (table 3) in group B and B+C are similar (152.7 cm and 153.9 cm). The maximum and minimum heights in group B were 172 cm and 140 cm and in group B+C were 178 cm and 139 cm.
The age groups (table 4) are comparable in group B and B+C with the maximum patients in age groups of 31-40 yrs and 61-75 yrs (29% each) and minimum patients in 41-50 yr (17%).
In both the groups (table 5), orthopedical surgeries constituted maximum with 54% (group B) and 49% (group B+C), respectively. All the surgical procedures are comparable in both the groups.
Figure 6
In our study (table 6), the mean time of onset of analgesia in group-B was 16+/- 3.34 (S.D) minutes and in group-B+C was 12.7+/-0.87 (S.D) minutes. The Statistical analysis by Student’s unpaired t-test showed that time of onset of analgesia in group-B+C was significantly less when compared to group-B (t = 4.1).
In the bupivacaine group (table 7), pain appeared as early as 60 minutes in 2 patients. At 1.5 hrs 3 patients, at 2 hrs 13 patients (35%), at 2.5 hrs 26 patients (75%), at 3 hrs 33 patients (95%) and by 3.5 hrs (100%) of patients experienced pain. In the bupivacaine and clonidine group, pain appeared at 3 hrs in 2 patients. At 3.5 hrs 6 patients (16%), at 4 hrs 24 patients (65%), at 5 hrs 30 patients (86%) and by 6 hrs 100% of patients experienced pain.
In the bupivacaine group (table 8), most of the patients were awake, alert (sedation score 1) and only 16-17% of patients were drowsy (sedation score 2) in between 45-90 minutes after epidural dose. No patient was found asleep (sedation score 3)
In the bupivacaine + clonidine group (table 9), after 15 min of drug administration, 29 patients (85%) were asleep (sedation score 3) and from 30min until 2 hrs 100% of patients were asleep (sedation score 3) and up to 70% patients were asleep at 3 hrs. By 4 hrs all the patients were awake and alert (sedation score 1).
From the table 10, we observe that the patients in Group B had fair (QOA 2 -40%) to good pain relief (QOA 3 – 46%) and the patients in Group B+C had good (QOA 3 – 54%) to excellent pain relief (QOA 4 – 35%).
From the table 11, it is observed that the incidence of nausea and vomiting was similar in both groups (14% in Group B as compared to 11% in Group B+C). 3 patients in Group B out of 35 had incidence of shivering (9%) while no shivering was observed in Group B+C. Dry mouth was observed in 7 patients (20%) and was significantly higher in Group B+C than Group B. Incidence of urinary retention was similar in both groups.
No incidence of bradycardia, hypotension or respiratory depression was observed in either group.
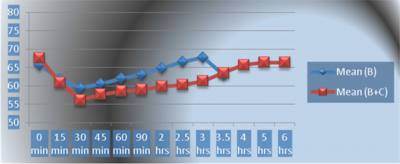
In comparison of group B and group B+C (graph 1), by using the unpaired student t-test, at the baseline VAS of two groups are similar. A highly significant difference in VAS was seen from 15 min until 3.5 hrs in between the groups.
In comparison of group B and group B+C (graph 2), by using the unpaired student t-test, at the baseline sedation score of two groups are similar. A highly significant difference in sedation score is seen from 15 min until 3.5 hrs in between the groups.
In comparison of group B and group B+C (graph 3), by using the unpaired student t-test, at the baseline SBP of two groups are similar. Significant decrease in the SBP was observed at 15min and highly significant decrease in SBP was seen from 30 min until 3.5 hrs in between the two groups. However, no incidence of hypotension was noticed in either group.
In comparison of group B and group B+C (graph 4), by using the unpaired student t-test, at the baseline DBP of two groups are similar. At 15 min no significant difference is noticed between the two groups. Highly significant decrease in the DBP was observed at 30 min and significant decrease in DBP was seen from 45 min until 2 hrs in between the two groups.
In comparison of group B and group B+C (graph 5), by using the unpaired student t test, at the baseline pulse rate of two groups are similar. At 15 min no significant difference is noticed between the two groups. Significant difference in pulse rate was seen at 2.5 hrs in between the groups. At all other times, there was no significant difference between the two groups.
:
In comparison of group B and group B+C (graph 6), by using the unpaired student t-test, at the baseline respiratory rate of two groups are similar. In between 2.5-3.5 hrs highly significant difference is noticed between the two groups. Significant difference in respiratory rate was seen at 60 min and 2 hrs in between the groups. At all other time, there was no significant difference between the two groups
Discussion
Clonidine is a selective partial alpha-2 adrenergic agonist with a selectivity ratio of 200:1 in favor of alpha-2 receptors. It is lipid soluble and easily penetrates BBB to reach the hypothalamus and medulla when injected epidurally. It stimulates inhibition of alpha-2 adrenoreceptors to reduce central neural transmission in the spinal neurons. Inhibition of substance-P release is also believed to be involved in analgesic effect4,5.
The alpha-2 adrenoreceptors are located on the afferent terminals of both peripheral and spinal neurons, on neurons in the superficial laminae of spinal cord and within several brainstem nuclei. The superficial laminae of dorsal horn contain 3 groups of neurons: tonic, adapting and single-spike-firing; all of which are important neuronal structures for pain transmission, receiving most of their primary sensory input from A delta and C fibres. Studies in rats show that clonidine partially inhibits voltage gated sodium and potassium channels and suppresses generation of action potentials in tonic firing spinal dorsal horn neuron. The analgesic effect of clonidine is more potent after neuraxial administration indicating a spinal site of action and favours neuraxial administration5,6.
Sedation is due to its action on locus ceruleus. Sedation after epidural clonidine is due to its systemic absorption and vascular redistribution to higher centres.
Clonidine affects blood pressure in a complex fashion because of opposing actions at multiple sites. In the nucleus tractus solitaries and locus ceruleus of brainstem, activation of post synaptic alpha-2 adrenergic agonists reduces sympathetic drive. It also activates non adrenergic imidazoline preferring binding sites in the lateral reticular nucleus, thereby producing hypotension and anti arrhythmic action6,7.
In the periphery, its action on presynaptic alpha-2 receptors at sympathetic terminals reduces the release of norepinephrine, causing vasorelaxation and reduced chronotropic drive. The brainstem and peripheral effects of alpha-2 stimulation are counter balanced by direct peripheral vasoconstriction through alpha-1 receptors6,7.
Clonidine causes a decrease in peripheral resistance, renal vascular resistance, heart rate and blood pressure. In the absence of profound hypotension, renal blood flow and glomerular filtration rate remain essentially unchanged6,7.
Clonidine alone does not produce profound respiratory depression even after massive overdose nor does it potentiate respiratory depression from opioids8.
After epidural administration clonidine is rapidly and extensively absorbed into spinal CSF compartment, with concentrations peaking 30-60 min after injection. The peak levels in arterial blood occur within 10min and in venous blood within 30-45 min. the correlation between clonidine concentration and analgesia is relatively poor. In contrast, there is strong correlation between CSF clonidine concentration and epidural analgesia7.
Clonidine is highly lipid soluble and readily distributes into extra-vascular sites including central nervous system. Clonidine’s volume of distribution is 2.1+/-0.4l/kg. The binding of clonidine to plasma protein is primarily to albumin and varies between 20-40% in vitro. In humans, clonidine metabolism follows minor pathways with the major metabolite p-hydroxyclonidine being present at less than 10% of concentration of unchanged drug in urine.
Our results matched with study done by Bonnet et al., who compared epidural and intramuscular clonidine (2ug/kg). The onset of analgesia in both clonidine groups was found to be within 15min and the duration of action in epidural clonidine group was 208+/-87min and the range of analgesic duration was 45-360 min9.
Our results also matched with study done by Bonnet Boica et al who compared epidural clonidine 150ug with epidural saline injection. In there study onset of analgesia was within 15min and they suggested high lipid solubility of clonidine to be responsible for its rapid action. They found that mean duration of analgesia in epidural clonidine was significantly longer (210min vs 45min). Better pain relief (satisfactory analgesia) was noted in epidural clonidine group. It was observed that following clonidine administration, all patients experienced drowsiness. Patients rested quietly in beds with eyes closed but were able to respond immediately and accurately. In their study, duration of drowsiness ranged from 141+/-38min and the duration of drowsiness corresponded with duration of analgesia. Also they concluded that presence of drowsiness neither compromised nor complicated VAS measurement as patients were able to measure their VAS whenever required. They concluded that maximum decrease in MAP is at 30 min of epidural clonidine injection and significant decrease in MAP is seen until 180 min10.
Eisenmach et al in there study of epidural clonidine analgesia following surgery compared 100-300 ug ; 400-700 ug and 700- 900 ug epidural clonidine. They concluded that sedation following any dose of clonidine was variable and lasted for 1-3hrs and was not dose dependent. They observed that with epidural clonidine 100-300 ug dose, MAP decreased maximally at around 47+/-4 min (range 15-90 min) and decrease was 21+/-4% from baseline. They observed that with epidural clonidine 100-300ug dose, no respiratory depression was observed as evidenced by no alterations in arterial PO2, PCO2 and oxyhemoglobin saturation11.
Mendez et al conducted a double blind, placebo controlled study to assess the efficacy, safety and appropriate dose of epidural clonidine for post cesarean section analgesia. 60 women were randomly assigned to three groups and received either bolus saline, 400 ug (5ug/kg) clonidine bolus or 800 (10ug/kg) bolus clonidine. They concluded that clonidine produced dose dependent sedation lasting for 3-4 hrs. They showed that both clonidine groups had lower blood pressures than the saline group from 2-12 hrs. No patient required treatment for hypotension. They suggested that maximum decrease in heart rate after epidural clonidine occurs 1-2 hrs of injection, at times of peak plasma concentration. concluded that groups did not differ in respiratory rate at any time, and no patient had a respiratory rate of <12 breaths per min There have been no reports of delayed hypotension or bradycardia from cephalad spread of epidural clonidine12.
We in our study preferred to use 150 ug clonidine (3-4ug/kg body weight) epidurally as some studies associated increased incidence of adverse effects like bradycardia, hypotension, and sedation with higher doses of clonidine. However, in our study patients only had dry mouth as the only significant adverse effect.
Limitations of the study includes, as pain is a subjective phenomenon associated with a wide variability of responses among the individuals, it is difficult to standardize the variable. What may be tolerable for one person may be intolerable for another person. Under these circumstances it is difficult to assess and grade the pain the same manner which can lead to a lot of unwanted bias. Also difference in type of surgery may also lead to variations in duration of analgesia. This can be negated in future studies by selecting similar type of patients undergoing same operative procedure.
Conclusion
Epidural clonidine with bupivacaine provides a rapid, excellent and longer duration of analgesia when compared to epidural bupivacaine. Significantly shorter time for onset of analgesia, significantly longer duration of analgesia with good sedation was seen in epidural clonidine + bupivacaine group as compared with epidural bupivacaine group. Also no incidence of hypotension, bradycardia and respiratory depression was seen in combination group. Dry mouth was the only side effect observed.
However, the duration of action of single epidural clonidine dose is too short for most of our patients (3-4hrs). Because of its relatively brief duration of analgesia, it may be necessary to infuse epidural clonidine continuously in order to produce complete analgesia of prolonged duration. Refinement of clonidine therapy and its ultimate usefulness compared to current therapies (patient controlled IV analgesia and epidural analgesia) has to be determined in future studies. Also studies can be done to compare epidural clonidine with opioids like fentanyl, buprenorphine and combination of low dose of clonidine and opioids for postoperative analgesia.