Pros and Cons of Transesophageal Echocardiography in Trauma Care
D Marciniak, C Smith
Citation
D Marciniak, C Smith. Pros and Cons of Transesophageal Echocardiography in Trauma Care. The Internet Journal of Anesthesiology. 2009 Volume 23 Number 2.
Abstract
Transesophageal echocardiography (TEE) is a well-established technology in anesthesiology and cardiology that is now becoming integrated into the management of trauma patients. Multisystem trauma alone is not a Class 1 indication to perform TEE, but acute hemodynamic stability is considered such an indication. There is demonstrated utility for its implementation in fresh trauma patients, during intraoperative management, and for directing care in the intensive care unit. Volume status, great vessel injury, cardiac lesions, and evidence of ischemia can be visualized quickly, thus assisting in directing treatment. TEE has several advantages and disadvantages when compared to other established diagnostic tools, such as pulmonary artery catheters, transthoracic echocardiography, and aortography , so its use must be considered on a case by case basis. While TEE has been shown to be safe, it is not without risk and carriers an overall morbidity of 0.2%. Studies conducted in trauma patients have not indicated any additional risk compared to other populations. TEE has an emerging role in acute and sub-acute trauma and wider implementation has the potential to improve patient care.Learning Objective: Discuss the advantages and limitations of transesophageal echocardiography (TEE) in trauma.
History
In 1881, the roots of echocardiography were discovered when the properties of piezoelectric crystals were first observed. When exposed to an electric field, these crystals vibrate and produce a sound. Over time, various instruments were developed to detect and utilize these sounds. During World War II, SONAR waves were used for underwater navigation and surface warfare. In the 1960s, transthoracic echocardiography in M, or ice pick, mode was the first medical utilization of this technology. As computer processing and miniaturization improved, the modern 2D real time imaging and omniplane transesophageal echocardiography (TEE) probes have revolutionized cardiac imaging. Echo is also used in other modern applications such as the FAST exam (focused abdominal sonography for trauma), solid organ imaging, peripheral nerve blocks, and vascular access.
Introduction
TEE is a well-established imaging modality in cardiac medicine and anesthesiology. A modern TEE probe is essentially a high frequency ultrasound transducer (usually 2.5 to 7.5MHz) mounted on the tip of directable gastroscope frame. Piezoelectric crystals are imbedded within the transducer. A typical probe can be placed into a patient as small as 25kg. 1 With topical mouth anesthesia and light sedation, an average patient can swallow the gastroscope without problem. Intraoperatively, patients are usually tracheally intubated and under general anesthesia and have no problem accepting the probe. Because the transducer lies in the lower esophagus in close direct contact with the posterior border of the heart, the images are superb since there is no interference by lung tissue.
2D and Doppler echocardiography are based on the reflections of high frequency sound waves from the heart and great vessels. With 2D imaging, the transducer emits a signal in brief pulses. After emission of the sound wave, the transducer becomes a receptor and waits for the signal to be reflected back by the structures along its pathway. Multiple scan lines are analyzed to produce a moving image with adequate temporal resolution. Optimal 2D images are obtained when the angle between the transducer and the imaged structure is close to 90 degrees. Spectral and color flow Doppler rely on measuring the difference between the initial known frequency and the backscattered signal returned from moving blood cells. The Doppler equation describes the relationship between change in frequency of the reflected signal and the velocity of the red cells. The simplified Bernoulli equation transforms velocities into pressure units. The 3 types of Doppler are continuous-wave (CW) pulsed wave (PW) and color Doppler.
Standard Exam
A standard comprehensive exam is comprised of 20 cross-sectional views. In the upper esophageal level (figure 1), the ascending aorta, main pulmonary artery, both atria and the aortic and pulmonic valves can be visualized. 2
Figure 1
From Feigenbaum's Echocardiography, Sixth Edition. Feigenbaum H, Armstrong WF, Ryan T. Lippincott Williams & Wilkins, Philadelphia, 2005.
At the mid-esophageal level (figure 2), both atria and ventricles along with the mitral and tricuspid valves can be observed.
Figure 2
From Feigenbaum's Echocardiography, Sixth Edition. Feigenbaum H, Armstrong WF, Ryan T. Lippincott Williams & Wilkins, Philadelphia, 2005.
The trans-gastric level (figure 3) allows imaging of both ventricles.
Figure 3
From http://www.med.yale.edu/intmed/cardio/imaging/techniques/echo_tee/index.html
CC Patrick J. Lynch and C. Carl Jaffe, Yale University, 2006.
Finally, the descending thoracic aorta and distal aortic arch can be visualized. (Figure 4) Of note, the distal ascending aorta and the proximal arch are not usually visualized with TEE because of shadowing from the left mainstem bronchus and trachea. 3
Figure 4
Indications
Class 1 indications, or indications supported by strong evidence or expert opinion and shown frequently useful in improving outcome include acute hemodynamic instability, an unstable intensive care unit (ICU) patient with suspected thromboembolism or valvular abnormality, and suspected thoracic aortic dissection/ aneurysm/ disruption who need immediate evaluation. 4 (Table 1)
Category 1: frequently useful in improving clinical outcomes and is often indicated depending on patient risk and practice setting. Supported by the strongest evidence or expert opinion
Category II: may be useful in improving clinical outcomes. Indications supported by weaker evidence and expert consensus.
Category III: appropriate indications are uncertain
Common lesions diagnosed by TEE include hypovolemia, thromboembolism, pericardial effusion, and trauma to the heart and great vessels. 5 Polytrauma alone is not a category one indication for TEE per se, but acute and persistent hemodynamic instability is considered such an indication. Class II indications are monitoring for myocardial ischemia, myocardial infarction, patients with increased risk for hemodynamic disturbances in the perioperative setting, patients with intra-cardiac foreign bodies, and intra-operative detection of air emboli.
Hypotension
Acute hypotension is a problem commonly encountered in trauma patients. TEE allows for evaluation of right and left ventricular function, preload, valves, and the great vessels. A common diagnosis in the trauma setting is hypovolemia with a hyperdynamic left ventricle secondary to blood loss. (Table 2)
Abbreviations: LV- left ventricle, RV- right ventricle, LA- left atrium, RA- right atrium, IVC- inferior vena cava, PA- pulmonary artery, E/A from transmitral flow, S and AR from pulmonary venous flow, E’ from tissue Doppler of the mitral annulus
It is a basic skill to evaluate if the ventricles are hyperdynamic or appear completely filled. Formal measurements can be made, such as estimation of left ventricle ejection fraction with the modified Simpson’s method of disks, but it relatively simple to evaluate gross function. In addition to volume status affecting hemodynamics, systolic function can be gauged quickly in the trauma setting. The fractional area change (FAC) of the left ventricular cavity can be used as a global index of systolic dysfunction. A measurement of the left ventricular cross sectional area is made during end systole (LVAs) and end diastole (LVAd) at the mid-papillary level (Figure 5). The FAC can be calculated with the following equation:
FAC=(LVAd-LVAs)/LVAd.
The normal range for the variable is 35-65%. The FAC at the mid-papillary level is also sometimes referred to as the 'Area Ejection Fraction'. 6
Figure 7
If there is a concern of ventricular dysfunction, TEE allows for evaluation of LV wall motion abnormalities in the basal, mid, and apical LV. This is particularly useful in patients with suspected myocardial contusion, ischemia, or stunning following blunt chest injury. In the setting of myocardial injuries, wall motion abnormalities precede EKG changes or a rise in cardiac enzymes. Traumatic valvular injury can also be diagnosed rapidly with TEE. Lacerations of valvular annuli and rupture of chordae sometimes occur in blunt chest injury and are difficult to diagnose in the initial stages of trauma resuscitation. TEE provides superb imaging of the valves and can be preformed while other resuscitative measures are taking place; it offers an early change in course for valvular lesions that might otherwise be difficult to diagnose. One study estimated the time to establish a diagnosis is as short as 11 minutes. 7
Cardiac Injury
Direct cardiac injury is one of many factors contributing to hemodynamic instability in the trauma patient. Regional or global pericardial effusions and tamponade can be easily visualized with TEE; this is especially valuable intraoperatively when the typical windows used with a FAST scan or transthoracic echocardiography (TTE) are obscured by the drapes or surgical field. Chamber collapse is used to guide the diagnosis of tamponade (Figures 6a and 6b).
Figure 6 A,B,C – The patient suffered multiple trauma from a car accident 10 days prior. She developed tachypnea, hypotension, and pulsus paradoxus. Transthoracic echo showed a large pericardial effusion with definite right atrial collapse (arrow, 6A- apical 4 chamber view) and marked left ventricular respiratory variation (6B- pulse wave doppler of the transmitral inflow). After pericardiocentesis and removal of 250 ml, signs of tamponade resolved (6C- apical 4 chamber view). Left heart contrast was then given without evidence of extravasation. Abbreviations: LV- left ventricle, RV- right ventricle, LA- left atrium, RA- right atrium, * pericardial effusion
The sensitivity of right atrial collapse is between 70 and 100% and the specificity is 80 to 100%. For the right ventricle, collapse is 60-90% sensitive and 80 to 100% specific. 8 TEE is often used to establish a diagnosis when TTE is inadequate and is more adept at visualizing regional areas of tamponade, especially that of the left atrium.
Pulmonary Embolus
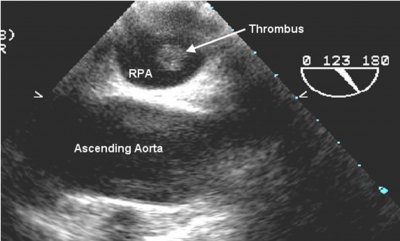
There is a rare potential to directly visualize large pulmonary emboli with TEE (Figures 7a and b).
Figure 11
Figure 12
However, the manifestations of right heart strain can be much more easily appreciated. Such findings may include right ventricular (RV) dilatation and/or hypokinesis, tricuspid regurgitation, pulmonary hypertension, and pulmonary artery or inferior vena cava dilation. 9 McConnell’s sign, which describes preservation of the RV apex but akinesis of the mid-RV free wall has a 77% sensitivity and 94% specificity for pulmonary embolism (PE). 10
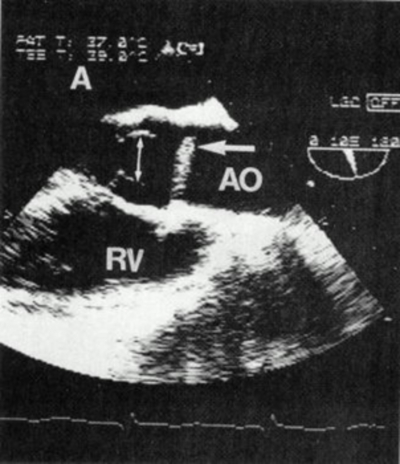
Left Ventricular Outflow Tract Obstruction
Left ventricular outflow tract (LVOT) obstruction with or without systolic anterior motion (SAM) of the mitral valve can also result in hypotension (Figure 8).
Figure 8 – Systolic anterior motion of the mitral valve (MV) and mitral-septal contact causing left venticular (LV) outflow tract obstruction. This condition may cause severe hypotension, especially in hypovolemic patients with hypertrophic cardiomyopathy. Hypotensive patients with SAM can be treated with volume and beta blockers which reduce systolic anterior motion and obstruction by decreasing early left ventricular ejection acceleration, decreasing the early systolic pushing force on the protruding mitral leaflet. From Wigle ED, Sasson Z, Henderson MA, et al. Hypertrophic cardiomyopathy. The importance of the site and extent of hypertrophy. A review. Prog Cardiovasc Dis 1985;28:1-83.
Patients with hypertrophic obstructive cardiomyopathy (HOCM) or subvalvular aortic stenosis, are at particular risk for cardiovascular collapse during traumatic injury. This cardiac lesion is made worse with tachycardia and low cardiac filling pressures. Restoring intravascular volume together with avoiding tachycardia are key in resuscitating these patients. TEE can help establish the diagnosis, but it can also aid in management of heart rate since there is hesitancy to use beta blocking drugs in hypotensive trauma patients. ICU management of HOCM patients will also be streamlined if the diagnosis is made early in the admission.
Prospective Studies Of TEE In Trauma
There is evidence to suggest an expanded role for TEE in trauma scenarios. A study by Mollod and Felner 11 demonstrated that 15 of 16 patients with chest trauma had findings that influenced a change in management, such as the timing and type of intervention, location of intracardiac foreign bodies, and optimization of medical management. They specifically found TEE useful in detecting and subsequently managing myocardial injuries, traumatic shunts, and aortic dissections. Catoire 12 evaluated two groups of multiply injured patients for mediastinal injuries. One group had a high index of suspicion for such injuries and another group did not have a high suspicion. New or interesting diagnoses were discovered in 70% of patients in the high suspicion group and 33% of patients in the low suspicion group. Myocardial and aortic injuries were either discovered or ruled out and pericardial fluid was observed in many patients. Ventricular dysfunction and severe hypovolemia were observed in several hemodynamically unstable patients. In all, 70% of trauma patients with thoracic or mediastinal injury revealed a new diagnosis. These authors concluded that “TEE is of the utmost importance in multiple injury patients … providing a safe and rapid examination of the mediastinal structures and an evaluation of the hemodynamic status.”
Blunt Aortic Injury
Aortic rupture is an extraordinarily lethal injury. A student by Richens 13 reviewed 132 cases of aortic rupture due to blunt chest injury in automobile accidents and found a 2% survival rate. TEE can rapidly diagnose such injuries by direct visualization of a dissection , the presence of an intimal or medial flap, gross thickening of the aortic wall by hematoma, or through evidence of intraluminal thrombus or debris at the injury site (Figure 9A and 9B).
Figure 13
Figure 14
This will ultimately lead to changes in management and save valuable time and patient exposure to inherent dangers of invasive studies or the even the perils of transport.
Penetrating Heart Trauma
In addition to blunt chest trauma, TEE has utility in penetrating cardiac trauma. Traumatic aortic fistulae 14 , ventricular lacerations 14 (Figure 10), and nail gun wounds (Figure 11) have been described. The advantage of using TEE in these scenarios is that an exact anatomic lesion can be isolated within minutes, allowing for more expeditious medical and surgical decision making. Cardiac function can also be evaluated post-repair to assist in determining if the lesion has subsided and the cardiac performance is adequate.
Figure 15
Figure 16
Intraoperative Cardiac Arrest
Cardiac arrest during intraoperative trauma surgery is often very challenging to reverse. A range of etiologies exists and there is minimal time to establish a definitive diagnosis. Recent evidence 14 suggests a valuable role for TEE in these situations. In a study reviewing 22 patients with hemodynamic collapse undergoing non-cardiac surgery, TEE was able to establish a diagnosis in 19 of these patients. Etiologies included PE in 9 patients, myocardial ischemia in 6, hypovolemia in 2, and tamponade in two. Fourteen of these patients survived their arrest and 12 had changes in management due to TEE. Utilizing TEE during perioperative arrests should be considered if available, as there is a strong indication of benefit.
Intensive Care (ICU)
TEE can provide benefit in the ICU. Frequently, patients are hemodynamically unstable due to under-resuscitation, sepsis, undiagnosed cardiac injury, or pulmonary embolism (PE figure). TEE provides a diagnosis in many instances and may be safer for the patient since they will not have to be exposed to invasive monitors such as pulmonary artery catheters, contrast media, or ionizing radiation. Since TEE can be done at bedside, the perils of transport are also eliminated.
TEE VS Pulmonary Artery Catheter
Pulmonary artery catheters (PACs) can provide continuous measurement of pulmonary artery (PA) pressure, frequent or continuous measurement of cardiac output (CO), filling pressures, and mixed venous oxygen saturation (SvO2). However, these values can be altered by positive pressure ventilation and ventricular non-compliance independent of LV preload. Data from TEE may differ significantly from a PAC, especially if there is pre-existing myocardial dysfunction, cardiomegaly, or right ventricular dysfunction. 15 TEE will give direct measurement of many of these values, where PACs are indirect. Most PAC values can be calculated with TEE except SvO2. A TEE exam is typically faster and may be more suited for an acutely hemodynamically unstable patient. Conditions such as cardiac tamponade may be better diagnosed with TEE because the fluid collection is directly visualized, where it is inferred with a PAC. 7 It is also important to consider that a PAC decreases the resuscitative capacity of the introducer it occupies and that may be a critical factor in a patient that emergently requires volume. 18 PACs have a rate of complication estimated at 1-5% where TEE is reported as 0.1-0.2%, 7 so there is a potential for increased safety with a TEE evaluation. (Table 3)
Modified from Mair, P, Vezinia DP, Sanchez, R. (2007). Transesophageal Echocardiography for Trauma and Critical Care. In Wilson, WC, Grande, CM, Hoyt, DB. In
TEE VS TTE
TEE and TTE can both be effectively used in trauma and there are advantages and drawbacks to both. Because TTE is a non- invasive test, it is usually employed initially. Harmonics and use of left heart contrast improve the quality of the TTE exam, especially in difficult to image patients. 18 However, TTE is still suboptimal in some patients due to obesity, overlying bandages and chest tubes, and the effects of positive pressure ventilation. Moreover, there is now a black box warning regarding the use of left heart contrast agents (Definity, perflutren lipid microspheres) due to the risk of anaphylaxis and death, although this risk appears to be very low (R. Finkelhor, personal communication). Positive pressure ventilation may make TTE evaluation of the valves, right ventricle, and the interatrial septum more difficult. This is not usually the case with TEE. Compared with TTE, TEE has greater sensitivity and specificity in evaluating valvular and aortic pathology, prosthetic valves, interatrial shunts, and cardiac sources of emboli. There is, however, more apical LV foreshortening with TEE. (Table 4)
Figure 18
Modified from Mair, P, Vezinia DP, Sanchez, R. (2007). Transesophageal Echocardiography for Trauma and Critical Care. In Wilson, WC, Grande, CM, Hoyt, DB. In
Complications And Contraindications To TEE
While the complication rate of TEE is low, it is not zero. Odynophagia or swallowing abnormalities are estimated to occur in 0.1% of cases, upper gastrointestinal (GI) hemorrhage 0.03%, esophageal perforation 0.01%, dental injury 0.03%, and endotracheal tube malposition 0.03%. (Table 5)
Absolute contraindications to TEE include esophageal pathology, recent upper GI surgery, perforated viscus, and a full stomach in a patient with an unprotected airway. Relative contraindications include hiatal hernia, chest irradiation, and atlanto-axial joint disease including an uncleared cervical spine. (Table 6)
In studies evaluating the use of TEE in acutely injured patients, no morbidity from the TEE examination was noted. 14 , 15 However, the decision to perform TEE on these patients must be made on a case-by-case basis with careful consideration of risk and benefit. If the patient is able to communicate, one should inquire about difficulty swallowing pills or food, and elucidate a history of esophageal or stomach surgery. If there is a concern, consideration should be given to esophageal imaging (endoscopy or barium swallow) prior insertion of the TEE probe. TEE should only be done by physicians experienced in the use of this modality. Training, certification, and credentialing in TEE are of obvious importance (Table 7).
Conclusion
In conclusion, TEE is a diagnostic and monitoring tool that can provide great benefit to the trauma patient. Its early consideration can have significant impact on patient care, but like all tools, must be used thoughtfully and cautiously.