Histopathological Profile Of Tumours Of Midgut And Hindgut—Five Year Study In Tertiary Care Hospital With Review Of Literature.
K Jhajj, N Sood, V Malhotra
Citation
K Jhajj, N Sood, V Malhotra. Histopathological Profile Of Tumours Of Midgut And Hindgut—Five Year Study In Tertiary Care Hospital With Review Of Literature.. The Internet Journal of Pathology. 2010 Volume 13 Number 1.
Abstract
This is a five year study of 400 cases of tumours of midgut and hindgut reported by pathology department in a tertiary care hospital. They were studied taking into consideration pathological findings and classification was done as per WHO guidelines. The study highlighted that hindgut tumours (large intestine & anal canal) were more common than midgut (small intestine) i.e. about ten times the midgut tumours along with male to female ratio of 2.2:1.The mean age of presentation of benign and malignant tumours was 32.6 years and 54.5 years respectively. Tubular adenoma was the most common benign tumour and adenocarcinoma was the most common malignant tumour and large intestine was the most common site for both of these tumours. But almost all kinds of tumours ranging from benign epithelial tumours to carcinoids even rare like Maltomas, Lipomas, FAP, Peutz Jeghers polyps, metastatic tumours and malignant mesenchymal tumours were observed and highlighted in the study.
Introduction
This study was conducted keeping in view that midgut and hindgut tumours had the highest incidence in our hospital. But when incidence of the tumours was compared between midgut and hindgut it was seen that tumours of midgut were very low where as major chunk was formed by hindgut tumours.One of the enigmas of medicine is the low incidence of neoplasms in small intestine in comparison to its length as these tumours comprising only 3-6% of all gastrointestinal tract tumours with slight preponderance of benign tumours.
As compared to small intestine colon and rectum are the leading sites for cancer in developed countries and in developing countries. Both environmental and genetic factors play a key role in the aetilogy. Genetic susceptibility ranges from a well-defined inherited syndrome e.g. familial adenomatous polyposis and some of the benign neoplasms like adenoma carry a high risk of the malignancy and act as precursor lesion for colorectal carcinoma and tubular adenoma was the most common benign tumour of our study. Along with colorectal carcinoma there is seen an increase in the incidence of squamous cell carcinoma in last 50 years due to increase in HIV infection.
Cure is strongly related to the anatomical site, which makes accurate staging very important tool. At present anatomic staging is the main stay of clinical decision making. An accurate history and pathological classification of tumours of midgut and hind gut acts as a useful guide in staging and grading the tumours and assessment of prognosis of tumours. Thus improving the mortality and morbidity of tumours of midgut and hindgut.
Review of Literature
Tumours of Midgut
Midgut has low incidence of primary tumours especially considering its size. Those that do occur are often related to genetic syndromes, especially familial adenomatous polyposis. Incidence of lymphomas and endocrine tumours is as frequent as carcinoma. Data from United States SEER program [1] for 1973 to 1987 show an age adjusted incidence rate for adenocarcinoma of small intestine of 0.4 per 100000 per year. Endocrine tumours are the next most common tumours of midgut with duodenal tumours amounting to 22% of all gastrointestinal endocrine neoplasms [2] where as the jejunoileal tumours account 23-28% of all gastrointestinal endocrine tumours; making this the second most common site for endocrine tumours following appendix [3,4].
Mesenchymal tumours account about 14% of malignant small intestinal tumours[1]. Since epithelial and mesenchymal tumours are uncommon in midgut, lymphomas constitute a significant proportion i.e.30-50% of all malignant tumours occurring at this site. Metastatic spread to the small intestine is more frequent than any other site in the gastrointestinal tract. Secondary carcinomas of the small bowel are as common as the primary carcinomas[5].
Most tumours occur in sixth to eighth decade, with male to female ratio 1.5: 1[6]. In series of 99 cases of endocrine tumours of the duodenum , males were more frequently affected with male to female ratio is 1.5: 1 with mean age of presentation of 59 years [range 33-90 years][6].Where as median age of manifestation is approximately 67 years for non mucinious Adenocarcinoma, Mucinous carcinoma and carcinoid. Endocrine tumours of lower jejunum and ileum are distributed more or less equally between males and females. Patients range in age from 3 rd to the 10 th decade with peak incidence in the 6 th and 7 th decade.[2,3,7,8].
Various etiologic factors involved in development of tumours of midgut are:
Chronic inflammatory bowel disease: It is the major factor in development of midgut adenocarcinoma. In particular, long standing Crohn’s disease with multiple strictures is associated with small bowel carcinoma[9,10]. Both ulcerative colitis and crohn’s disease are both recognized as risk factors for NonHodgkin lymphoma at this site. Crohn’s disease is more often implicated in the development of lymphoma in midgut.[11].
Coeliac disease: It is another recognized etiological factor for small bowel carcinoma[12, 13, 14].
Miscellaneous causes: There is some epidemiological evidence that cigarette use and alcohol consumption are also risk factors[15]. Carcinoma a can develop in ileostomies in patients with ulcerative colitis or familial adenomatous polyposis subsequent to colonic metaplasia and intraepithelial Neoplasia in the ileostomy mucosa[16, 17].Approximately 15% of carcinoid tumours of the small intestine are associated with non carcinoid neoplasms, most frequently adenocarcinoma of the gastrointestinal tumours [18,19] supporting the hypothesis that secretion of growth factors is involved in their etiopathogenesis.
An increase incidence of lymphoma has been associated with both acquired and congenital immunodeficiency, iatrogenic immunodeficiency associated with solid organ transplantation and AIDS [20].In general lymphomas associated with immunodeficiency show a predelictation for extra nodal sites, particularly gastrointestinal tract.
Genetic factors:Patients with hereditary nonpolyposis colorectal cancer (HNPCC) and germ line mutations of hMSH2 or hMLH1 have an approximately 4% lifetime risk of small bowel cancer, which exceeds the risk of normal population 100 fold. In Peutz-Jeghers syndrome, the most common site of polyps is in the small intestine, and 2-3% of patients are at risk for developing intestinal carcinoma. Genes mutated in germline of patients with inherited syndromes that predispose to small bowel Neoplasia (APC, hMSH2, hMLH1, LKB1 and Smad4) may therefore play a role in the genesis of these tumours.
Tumours of Hindgut
An estimated 875000 cases of colorectal cancer occurred worldwide in 1996, representing about 8.5% of all new cancers [21]. According to the U.S. SEER database, the incidence rate of Adenocarcinoma of colon is 33.7/100,000 and increased by 18% during the period from 1973 through 1987 while incidence of rectal Adenocarcinoma (12.8/100,000) and mucinous Adenocarcinoma in the colon and rectum ( 0.3 and 0.8, respectively) remained relatively constant[1]. Incidence increases with age [22] carcinomas are rare before the age of 40 years except in individuals with genetic predisposition or predisposing conditions such as chronic inflammatory bowel disease.
Incidence rates in the 1973-87 SEER data for colonic and rectal Adenocarcinoma for males were higher than those for females [1]. The tumours of anal canal mainly squamous cell carcinoma are rare disease, but have shown a remarkable increase in incidence during past half century [24]. Tumours mainly affect patients in their 6 th and 7 th decade of life [24].But increase incidence are seen in male population and homosexual men appear to constitute a group at particular risk [25].
In a recent series, carcinoids from caecum to transverse colon (midgut) represented about 8% and descending colon and rectosigmoid (hindgut) carcinoids about 20% of 5973 gastrointestinal carcinoids. Rectal Carcinoids had a reported incidence of 0.14-0.76 cases per 100,000 populations per year .As compared to carcinomas and carcinoids lymphomas account about 0.2% of all neoplasms at this site. Mucosa – associated lymphoid tissue [MALT] lymphomas account for majority of lymphomas of the colorectum [11]. Sarcomas accounted for 0.1% of malignant large intestinal tumours in SEER data [1]
Various etiologic factors involved in development of tumours of midgut are:
Diet and life style: A high incidence of colorectal carcinomas is observed in populations with western type of diet .Epidemiological studies have indicted that meat consumption, smoking and alcohol consumption are risk factors. Inverse association includes vegetable consumption, prolonged use of non steroidal anti inflammatory drugs and physical exercise [21,22].
Chronic inflammatory bowel disease: they are the important aetiologic factor in the development of adenocarcinomas[26]. Population based studies show a 4.4 fold increase in mortality from colorectal carcinoma in patients suffering from ulcerative colitis. In clinical studies, the increase in incidence is usually higher, up to 20-fold[26]. Miscellaneous Factors: human papilloma viruses are the major infective organisms in development of squamous cell carcinoma of anal canal[25]. Increase incidence of hindgut tumours is associated with HIV.
Genetic Factors: The development of most colorectal carcinomas is believed to begin in a colorectal epithelial cell with a mutation and inactivation of APC (adenomatous polyposis coli) suppressor gene .This leads to various clonal mutations and their accumulation occurs i.e. activation of proto-oncogene such as c-myc and ras and inactivation of additional suppressor genes. . Some colorectal cancers are distinguished by extensive nucleotide insertions or deletions in numerous, unstable repeated sequences in tumour DNA, termed microsatellite instability [MSI].
Staging and Grading
Colorectal carcinomas are the most common malignant tumours seen in this study so staging and grading is very important from diagnostic and prognostic point of view. The classification proposed by C. Dukes in 1929-35 for rectal cancer serves as template for many staging systems currently in use. Now days Astler Coller classification is used. This classification based on depth of penetration into the wall and the presence or absence of metastasis in regional lymph nodes.
ASTLER AND COLLER STAGING OF TUMOURS OF COLON
A: tumour limited to the mucosa
B-1: tumor involving the muscular is external but not penetrating it
B-2: tumor penetrating through muscularis externa
C-1: tumours confined to the bowel wall but with nodal metastasis
C-2: tumours penetrating through the wall with nodal metastasis
D: distant metastasis
The percentage of tumour showing gland like structures can be used to define the grade. Well differentiated (grade1) lesions exhibit glandular structures in >95% of the tumour; moderately differentiated (grade 2) Adenocarcinoma has 50-95% glands; poorly differentiated (grade 3) has 5-50% and undifferentiated (grade 4) carcinoma has <5%. Mucinous Adenocarcinoma and signet ring cell carcinoma are considered poorly differentiated (grade 3). Medullary carcinoma is considered grade4.
Materials and Methods
The present study is a five year study (three years retrospective and two years prospective) in which all the specimens of tumours of midgut and hindgut received in the department of Pathology were analyzed with reference to light microscopic findings with special emphasis on the histological type and grade of tumours.
In each patient the clinical findings (age, sex, clinical presentation, and operative findings) were obtained from the medical records. Pathological findings (size, histologic subtype, architecture, vascular, lymphatic, perineural invasion, Astler Coller grade, stage, lymph node involvement) were obtained by examination of hemotoxylin and eosin- stained slides and from information in pathology reports. Histological subtypes were classified according to WHO classification of tumours of small intestine, large intestine and anal canal.
Observations
This was a five year study where 400 cases were studied. Large intestinal tumours formed the major part with the percentage of 90% followed by small intestinal tumours, which were 9.8% of all the cases, and lastly tumours of anal canal that constituted 1.2% of all cases (table no.1).
The tumours were divided into benign and malignant. The malignant tumours far exceeded the benign tumours in the present series. Out of the total 400 cases 344 were malignant and 56 were benign. The most common age group affected by the tumours was between 50- 59years (23.75%) with mean age of presentation being 54.5± 2.4 years. Youngest was a child aged one year and oldest was 92 year old.
In benign tumours the mean age of presentation was 32.6 years and in malignant tumours it was 54.4 years. The male to female ratio of all tumours came out to be 2.2:1. In the present study the most common clinical presentation was bleeding per rectum (25%) followed by obstruction (22.2%), perforation (2.5%), altered bowel habit (5.5%) and jaundice (3.8%). But majority of patients were asymptomatic.
The tumours were broadly classified as benign and malignant tumours. In the category of benign tumours tubular adenomas topped the list with a percentage of 40.8% followed by juvenile polyps (37.5%) (table no.3). In the category of malignant tumours adenocarcinoma were the most common tumours with the total of 82.6%, followed by Mucinous carcinoma (8%), Non Hodgkin’s lymphoma (2.9%) (table no.4).
In comparison of tumours both benign and malignant according to site it was found that large intestine was most common site for adenomas and carcinomas but mesenchymal tumours and carcinoids were more commonly seen in small intestine (table no. 5&6).
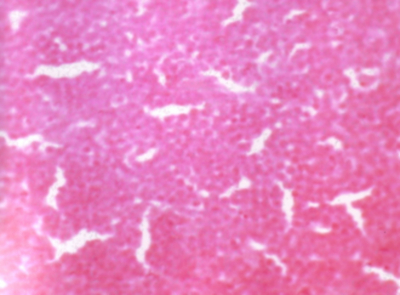
In small intestine the most common tumour was adenocarcinoma (46.2%) followed by Non Hodgkin’s Lymphoma (23.1%) (Figure No. 1), GIST (17.9%) (Figure No. 2), carcinoid (7.7%) (Figure No. 3) and Peutz Jegher’s polyp (5.1%) (Figure No. 4). Adenocarcinoma (Figure No. 5) occurred mainly in the periampullary region. There were 18 cases of adenocarcinomas of small intestine with mean age of presentation being 55.5 years and male preponderance (M: F 2.4:1).They were graded on the basis of glandular differentiation. 94.58% were moderately differentiated only 5.42% of cases were well differentiated. All the tumours had extended through the gut wall with regional lymph node involvement in 79.4% of the total cases. Rest of the cases showed reactive hyperplasia. In one case lymph node showed granulomatous inflammation with caseous necrosis which indicated the coexistence of tuberculosis, which is common in this part of world. No distant metastasis was seen.
There were total 9 cases of Non Hodgkin’s Lymphoma all of which were Maltomas and were graded as high and low grade as per WHO grading of Maltomas. Low grade Lymphomas were common (66.7%) as compared to high grade ones.
There were 7 cases of GIST. Majority of cases (71.4%) of GIST turned out to be low risk tumours with 14.3% cases intermediate and high risk GIST .Only two cases of benign tumours were seen in the small intestine. Both were males with mean age of presentation 22.5 years.
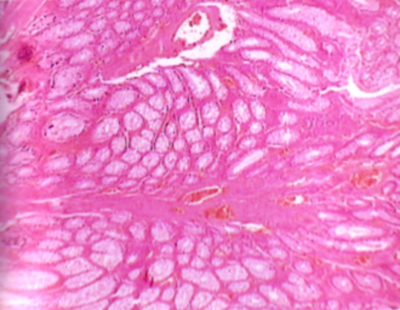
Figure 12
In large intestine malignant tumours were more common than their benign counterparts as 302 cases were malignant where as only 54 cases were benign. In benign tumours the mean age of presentation was 32.6 years and in malignant tumours it was 54.5 years with male to female ratio of 2.7:1. In large intestine the commonest benign tumour was tubular adenoma (42.8%) (Figure No. 6) followed by juvenile polyp (38.9%) (Figure No.7). In the category of malignant tumours adenocarcinomas were the commonest tumours (88.4%) followed by mucinous carcinoma (9.3%) and among adenocarcinomas mucin secreting adenocarcinomas (Figure No.8) were most common.
Staging of adenocarcinomas of colon and rectum
Staging of adenocarcinomas was done according to Astler Coller staging system. This staging was applied to large specimens i.e. colectomy specimen and abdominal perineal resection which constituted total 167 cases. In this staging system extent of tumour into the wall of gut and lymph nodes status, distant metastasis and grade i.e well differentiated, moderately differentiated and poorly differentiated (Figure No. 9,10&11) was documented.
The most common stage was B2 (52.7%) followed by C2 (46.7%) implying that nodal metastasis was seen in 46.7% of cases.
Mucinous carcinoma(Figure No.12) was the second most common malignant tumour after adenocarcinoma. Most common stage was C2 (64.7%) followed by B2 (35.7%) thus stating that lymph node metastasis was seen in majority of cases.
In case of anal canal all tumours were malignant with squamous cell carcinoma being most common (80%).
Discussion
This was a 5 year study conducted in a tertiary care hospital. All the specimens of midgut (small intestine) and hindgut (large intestine and anal canal) tumours submitted in department of Pathology were analyzed by light microscopic findings with special emphasis on the histological type and grade of tumours. Classification of tumours was done as per WHO guidelines. [23]
In the present analysis midgut tumours were less common (9.8%) in comparison to the tumours of hindgut (91.8%). The low incidence of small intestinal tumours is also in concordance with a population –based study of the incidence of malignant small bowel tumours done by Chow S,Chen CC et al and Rosai J, Ackerman [27,28] , who analyzed that small bowel tumours occurred rarely and they were 40 to 60 times less common than the large bowel tumours. A higher incidence was seen in the males irrespective of the type and the site of the tumour with M: F ratio of 2.2:1. This correlated with study done by Thomas RM, Sobin LH[1]. They analyzed 194452 cases of gastrointestinal tumours over the period of five years and found a M: F ratio of 2:1.
The most common age group affected was between 50- 59years with mean age of presentation being 54.5± 2.4 years. This is collaborated by studies done by Burke AP, Sobin LH et al and Solcia E ,Capello C, et al [2, 6] who reported that the mean age of presentation of the tumours of midgut and hindgut was 59 years (51-69 years).
Tubular adenoma was the most common benign tumour which is in concordance with study done by Rudy DR, Zdon MJ [30] who reported that the incidence of tubular adenoma was 83% of all the benign tumours.The most common malignant tumour was adenocarcinoma(82.6%).Various studies done by Berg JW, Howel MA, Rosai J, Ackerman & Kumar V, Abbas AK, Fausto N[28,29], found that adenocarcinomas were the commonest malignant tumour particularly in the duodenum and colon representing 70% of all malignant tumours in gastrointestinal tract. This is in concordance with our study.
Neuguet Al, Jacobson JS , et al and Chow J S,Chen CC et al [15] suggested that high incidence trends of adenocarcinomas occurring in the duodenum and the colon were due to similar risk factors in these regions. These studies showed that the risk factors for small bowel cancer include dietary factors similar to those implicated in large bowel cancer, cigarette smoking, alcohol intake, and other medical conditions, including Inflammatory Bowel Disease and familial adenomatous polyposis.
In the small intestine duodenum (58%) was the most common site to be affected by the tumours followed by ileum (25%) and jejunum (17%). This is in concordance with population based studies done by Chow JS,Chen CC et al[27] who observed that the small intestinal tumours were distributed proximally i.e.more in the duodenum.
However Ioannis Hatzaras et al. [31]observed that the most common location of small-bowel tumors was the ileum (374 cases; 29.7%), followed by the duodenum (320 cases; 25.4%) and the jejunum (193 cases; 15.3%). This disparity could be explained by the fact that in this study maximum cases were of the lymphomas. Whereas in our study adenocarcinomas were the commonest tumour and duodenum was the commonest site.
In the population based studies done by Chow S,Chen CC et al and Hatzaras I,Palesty A et al [27] adenocarcinomas were the most common tumours in the duodenum. They analyzed four major histologic types of cancer of the small intestine: carcinomas, malignant carcinoid tumors, lymphomas, and sarcomas. These varied considerably with regard to their proportional distribution among the subsites of the small intestine. Carcinoid tumors, lymphomas, and sarcomas rarely occurred in the duodenum, whereas nearly half of the carcinomas were found there. 87% of carcinoid tumors and 60% of lymphomas occurred in the ileum. This is in concordance with our study.
The second most common tumour observed in small intestine was Non Hodgkin’s Lymphoma (23.1%). In contrast a very low incidence was noted in large intestine (0.3%). This is in concordance with Rosai J , Ackerman [28] who found that small intestine was the common site for Non Hodgkin’s Lymphoma whereas they were rare in large intestine.
In our study all the lymphomas were Maltomas. Ileum was the commonest site of occurrence. Isaacon P, Spencer J, [33]analyzed that small-intestinal lymphomas were most often found in the ileum followed by duodenum and jejunum .Histopathologically majority of the intestinal lymphomas involving the small bowel were Maltomas.This is in concordance with our study. After lymphomas the next common tumour of small intestine was GIST (17.9%). This is collaborated by the study, done by Meittinen M, Saralomo RM, Lasato J[34], who reported that GIST was the most common mesenchymal tumour of small intestine and formed 14% of all the malignant small intestinal neoplasms.
In the present study large intestinal tumours, were broadly divided as benign (15.2%) and malignant (84.8%). Malignant tumours carried a very high incidence and were five times more common than the benign tumours. In the category of benign tumours, adenomas topped the list with commonest being tubular adenoma. The size of tubular adenomas ranged from 0.3-1.2 cms. The importance of size lies in the association with frequency of malignant transformation. According to the 2002 Willmar Cancer Center report [35] the frequency of cancer in adenomas less than 1 cm was one to 3%; in those between 1-2 cm, 10%; and in those more than 2 cm, more than 40%. This correlation could not be documented as most of the cases were lost to the follow up.
All the tubular adenomas diagnosed in our study were solitary except 2 cases which on colectomy specimen showed more than 100 polyps carpeting the entire the specimen ranging from 0.5-2 cms in size- these were diagnosed as FAP ( Familial adenomatous Polyposis). Both cases were seen in males with age of presentation 27.5 years. Rosai J, Ackerman [28] documented that tumours in Familial Polyposis manifested in second decade of life and occurred predominantly in males .This collaborated with our study.
Non Neoplastic polyps formed the next common category of benign tumours and the commonest polyp was Juvenile polyp (retention polyp) (38.9%). In 80.9% of these cases the mean age of presentation was 4.7 years with M:F ratio of 2.5:1. The remaining 9.1% of cases were seen in adults with a mean age of presentation 33.6 years and male to female ratio of 5:1. This is in accordance with Rosai J, Ackerman [28] who observed that juvenile (retention) polyp was the most frequent polyp seen in children but approximately one third of all the cases occurred in adults.
Adenocarcinomas were the commonest malignant tumours (88.4%) with mean age of presentation being 54.5 years and a male preponderance (male: female 2.5:1) that is collaborated by study done by Thomas and Sobin [1] that stated males had higher incidence rates for adenocarcinoma than did the females but the median age was slightly higher i.e. 70 years. Youngest age of presentation in our study was 14 years. He had no history of carcinoma in any of his family members.
Higher incidence of adenocarcinomas was seen in proximal colon (55.6%) as compared to distal colon (44.4%). Demers Y and Severson RK et al. [36] reported that contact time of faecal stream was higher in proximal colon as compared to distal colon & rectum due to slower faecal transit time. This explained the higher incidence of adenocarcinomas in the proximal colon. 2.3% of adenocarcinomas showed synchronous presence of tubular adenomas which is in concordance with study done by Eide TJ et al. [37] who reported that the large bowel specimens with carcinomas had higher incidence of polyps elsewhere in the specimen than those without carcinomas. Only 0.7% of adenocarcinomas showed association with inflammatory bowel disease particularly with Ulcerative Colitis, which is collaborated by Rosai J, Ackerman [28] according to which 1% of colorectal carcinomas were associated with ulcerative colitis.
Adenocarcinomas were graded into 4 major groups as per WHO guidelines. The most common grade was 2 (moderately differentiated) constituting 89.9% of all adenocarcinomas followed by grade 3 (8.2%) and grade 1(1.9%). This is collaborated by WHO [23] which identifies moderate differentiation as the commonest grade.
Adenocarcinomas were staged according to Astler Coller staging system. None of tumours presented with stage A whereas the most common stage of tumours was B2 (52.7%) followed by C2 (46.7%) and B1 (0.6%). This indicated regional lymph node involvement in 46.7% of the tumours. This is in accordance with study of gastrointestinal tumours done by Thomas RM, Sobin LH[1]. They analyzed 194452 cases of gastrointestinal tract tumours over the period of five years and found that almost fifty percent of adenocarcinomas showed regional lymph node metastasis at the time of presentation.
Mucinous carcinoma was the second most common malignant tumour of the large intestine. Various studies done by Thomas RM, Sobin LH, WHO & Sasaki O and Atkins et al.[1], also reported that mucinous carcinoma was the second most common type of carcinoma of large intestine. Mucinous carcinomas were staged on the basis Astler Coller staging system. The commonest stage was C2 (64.3%) indicating the presence of nodal metastasis. All other types of carcinomas (signet ring cell, undifferentiated, squamous carcinoma) formed less than 1 % of all the malignant tumours of large intestine so no conclusive opinion could be given.
Malignant mesenchymal tumour and Non Hodgkin`s Lymphoma together constituted 1% of the total malignant tumours of large intestine.This is in concordance with studies done by Thomas RH, Sobin LH and Roth SI, Helwig EB[1] who reported that carcinomas were the commonest malignant tumours of large intestine whereas lymphomas and sarcomas comprised only 1% of all the neoplasms.
In the present study only 5 cases were reported in the anal canal forming 1.25% of all tumours. This is in concordance with study done by Winawer SJ et al. [38], who reported that tumours of anal canal were rare. The male to female ratio of anal canal tumours in this study was 4:1. This is in variance with studies done by Winawer SJ, Fletcher RH, et al and Frisch M et al[38], who observed that there was female preponderance. However an increase in incidence was seen in male population. The relative disparity could be explained as admissions of male patients in the hospitals were more due socio economic setup of the state.
Most common tumour of anal canal was Squamous Cell carcinoma (80%) with mean age of presentation being 62.5 years. This is in concordance with study done by Thomas RM , Sobin LH [1] who noted that Squamous cell carcinoma was the commonest tumour of anal canal (75%) with mean age of presentation being 63 years.
Conclusion
This was a 5 year study conducted in a tertiary care hospital. 400 cases of tumour of midgut and hindgut were studied taking into consideration pathological findings and classification was done as per WHO guidelines. This study highlighted following features. Hindgut tumours (large intestine & anal canal) were more common than midgut (small intestine). They were ten times the midgut tumours. A higher incidence was seen in males with M: F 2.2:1. The mean age of presentation of benign and malignant tumours was 32.6 years and 54.5 years respectively. Out of all the tumours analyzed tubular adenoma was the most common benign tumour and adenocarcinoma was the most common malignant tumour. Astler Coller Stage B2 was the commonest Stage. But all types of tumours were encountered like FAP, Lipomas and metastatic tumours.
Acknowledgment
My sincerest thanks to Dr. Samarjit Kaur Sandhu, Dr. Navtej Singh and Dr. Sarita Nibhoria for their constant encouragement and help.