Posterior scleritis mimicking indirect carotid-cavernous fistula
T Kah, M Premsenthil, M Salowi, A Thanaraj, I ak Gudom
Keywords
indirect carotid-cavernous fistula, posterior scleritis, t-sign
Citation
T Kah, M Premsenthil, M Salowi, A Thanaraj, I ak Gudom. Posterior scleritis mimicking indirect carotid-cavernous fistula. The Internet Journal of Ophthalmology and Visual Science. 2008 Volume 7 Number 1.
Abstract
Purpose: To report a case of posterior scleritis that mimicked indirect carotid-cavernous fistula. Case Report: A 53 year old lady presented with two weeks’ history of right eye redness and blurring of vision associated with right sided headache and ocular pain. The episcleral vessels were dilated and tortuous. Fundus examination revealed optic disc swelling and choroidal folds. B-scan ultrasonography demonstrated the “T” sign which is diagnostic of posterior scleritisConclusion: This case report highlighted the variable clinical symptoms and signs of posterior scleritis. Clinician must maintain a high index of suspicion for posterior scleritis in patients who present with painful blurring of vision. Effort should be made to rule out any systemic association which must be treated promptly.
Introduction
Posterior scleritis is an uncommon manifestation of scleritis which may result in blindness. Diagnostic confusion may arise due to its variable clinical signs and symptoms 1. We report a case of posterior scleritis that mimicked indirect carotid-cavernous fistula.
Case Report
A 53 year old lady presented with sudden onset of right eye redness associated with two weeks’ duration of blurring of vision. The blurring of vision was preceded by right sided throbbing headache and ocular pain which increased in severity and waked the patient from her sleep. They were no precipitating, aggravating or relieving factors.
The associated redness was diffuse and increased gradually. The blurring of vision was gradual and progressive. She has no history of head or ocular trauma, eye discharge, photophobia, diplopia, flashes or floaters. Her left eye was unaffected. Systemic review was not significant. She has severe gastritis and had en episode of upper gastrointestinal bleed six months ago when she presented with melena. She is currently taking oral ranitidine 150 mg twice daily. There was no other past medical, ocular, surgical or drug history.
On examination, the visual acuity (VA) of her right eye was 6/60. The best corrected visual acuity (BCVA) was still 6/60. The near vision of her right eye was N48. The BCVA of her left eye was 6/6 with near vision N6. There was no strabismus. In ambient light, the right pupil was 5 mm while the left pupil was 3 mm (Figure 1). Relative afferent pupillary defect (RAPD) was positive on the right eye.
Figure 1
The right periorbital region was swollen. There was no obvious proptosis. The episcleral and scleral vessels were dilated. One of the dilated vessels (green arrow) had corkscrew appearance but the finer vessels were less tortuous. The conjunctiva was not chemotic and the underlying sclera was white (Figure 2).
Figure 2
Using Hertel exophthalmometer, the interpupillary distance was 110 mm, the position of the right corneal apex measured 16 mm while the left corneal apex measured 15 mm. The red reflex was present and equal in both eyes. Extraocular movements were unrestricted and there was no pain during ocular movement. The globe was not tender on palpation. There was neither thrill nor bruit. The cornea was clear. The anterior chamber was quiet and deep. The intraocular pressure was 14 mm Hg. Gonioscopy showed that the angles were widely open and there was no blood in the Schlemm canal.
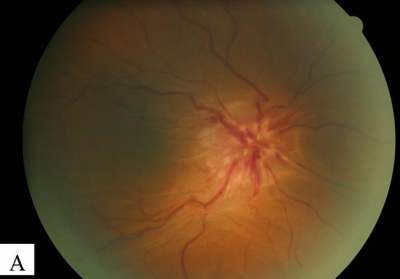
Funduscopy of the right eye showed that the optic disc was swollen and hyperemic. Disc hemorrhages were present at 2, 4, 6 and 10 o’clock position. Retinal veins were dilated and tortuous. Retinal arteries were tortuous but not dilated. Spontaneous venous pulsation was absent. There were prominent choroidal folds which were seen more obviously with the red free light. The macula was involved with the loss of foveal reflex (Figure 3). A flamed shaped hemorrhage was seen below the superior temporal arcade. There were no cotton wool spots, retinal edema, hard exudates, retinal or choroidal detachment and no choroidal mass.
Figure 3
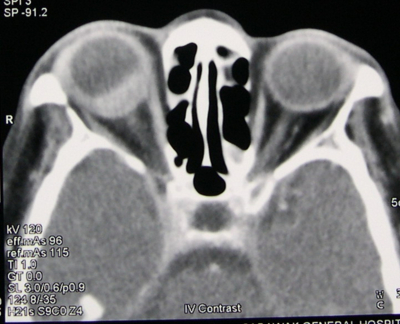
The patient was initially thought to have right indirect carotid-cavernous fistula. We ordered an urgent CT orbit and brain (Figure 4). The right globe was proptosed with uveal thickening which was most pronounced in the posterior wall. The lesion enhanced homogenously with intravenous contrast agent. The medial and lateral recti were thickened as well. The retro-orbital fat was normal, there was no retro-orbital tumor, the cavernous sinus was not enlarged and there was no dilatation of the superior ophthalmic veins.
Figure 5
B-mode ultrasonography showed diffuse thickening of the choroid, sclera and episcleral tissues. The thickness of the sclera-choroid complex measured 2.64 mm. The optic disc was swollen. There was fluid in the subtenon space producing a prominent T-sign (Figure 5). There was neither scleral nodule nor retinal detachment. The orbital veins were not dilated or tortuous. The T-sign was diagnostic of posterior scleritis.
Figure 7
Her blood results were negative for antinuclear antibody, rheumatoid factor and LE cells. Her ESR at presentation was 109 mm/1st hour. Urinalysis was normal.
The final diagnosis was right diffuse posterior scleritis with associated mild diffuse anterior scleritis and orbital myositis. There was no identifiable underlying systemic disorder associated with her posterior scleritis. The patient was informed of the treatment options and the possible side effects keeping in mind that she had a recent episode of upper gastrointestinal bleed. We decided to start with oral ibuprofen 400 mg four times daily and reviewed her after three days. Oral prednisolone was to be started if there was no improvement. She was also referred to a rheumatologist for co-management.
After three days, the patient achieved rapid symptomatic improvement. The headache and ocular pain disappeared resolved. At one week follow-up, the eye was no longer red and the vessels were not tortuous anymore. It was evident that the tortuous vessel seen during initial presentation is inherently corkscrewed. The optic disc swelling, retinal vessels tortuosity and choroidal folds reduced markedly (Figure 6). Her ESR was 25mm/1st hour.
Figure 8
The patient did not report any exacerbation of her gastritis nor did she develop any upper gastrointestinal bleed. Judging from the clinical response and decrease in ESR, we continued the oral ibuprofen 400 mg four times daily for another month without adding oral prednisolone. The rheumatologist was unable to elicit any systemic association and there was no other medication prescribed for the condition.
At one month, her vision was still 6/60. We decided to stop the oral ibuprofen as there were no more pain and signs of any inflammation. At two month, her vision was no light perception (NLP). She developed optic atrophy and the choroidal folds disappeared. B scan ultrasonography showed a hyperechoic lesion at the optic nerve head due to gliosis. The thickness of the sclera-choroid complex was 1.82 mm (Figure 7).
She was followed up three monthly for six months and six monthly for two years. At two year follow up, she remained asymptomatic. Her left eye was unaffected. There was still no evidence of any connective tissue or systemic diseases. Her ESR was 10 mm/ 1st hour and she was negative for LE cells and antinuclear antibody.
Figure 10
Discussion
Posterior scleritis, defined as sclera inflammation posterior to the equator, is an uncommon manifestation of scleritis. Posterior scleritis may occur in isolation, in which case diagnosis may be difficult 2. This patient initially presented a diagnostic challenge to us as the dilated episcleral vessels appeared corkscrewed. This raised the suspicion of an indirect carotid-cavernous fistula. The inherent corkscrew appearance of the large episcleral vessel was noted with the resolution of vascular congestion after treatment (Figure 6A). The vascular congestion was due to mild diffuse anterior scleritis. The combination of mild diffuse anterior scleritis, choroidal folds and optic disc swelling were valuable clues that led to the prompt work up for posterior scleritis.
Scleritis is known to be associated with systemic diseases. Rheumatoid arthritis is the most common systemic disease in association with posterior scleritis, followed by other connective tissue diseases and systemic vasculitides 3. Scleritis may be the presenting clinical manifestation of a systemic disease. Our patient had no evidence of systemic association although she had been on follow up for more than two years. Nevertheless, we kept in mind that scleritis is a barometer of systemic disease. Patients with connective tissue disease and systemic vasculitides may have ocular manifestation well in advance of definitive establishment of the diagnosis. Failure to acknowledge this point may result in delayed diagnosis and consequent permanent disability because of this delay 4.
B-mode ultrasonography is the most useful investigation modality for posterior scleritis. Highly reflective echoes with thickening of the uvea and sclera are usually present. B-scan ultrasound is useful in quantifying scleral thickness. The “T” sign is considered virtually diagnostic of posterior scleritis 5. The “T” sign is due to scleral edema in association with fluid within Tenon’s space. This results in a “T” shaped echolucent region just posterior to the sclera.
Oral non-steroidal anti-inflammatory drugs (NSAIDs) is the first line of treatment for scleritis 6. Treatment response usually becomes evident within 2 to 3 weeks. Our patient achieved marked symptomatic relief, reduction in clinical signs of inflammation and ESR within 1 week. In other cases, treatment failure with oral NSAIDs requires systemic corticosteroids alone or in conjunction with other immunosuppressive agents. Taking this into account and the fact that she had a recent episode of upper gastrointestinal bleed, we did not prescribe oral prednisolone. This decision was made with the best intention as the patient was fully informed of the risk and benefit of oral prednisolone.
Vision is almost always affected in posterior scleritis 2. It was very unfortunate that the patient has NLP despite the apparent clinical response to oral ibuprofen.
This case report highlighted the variability in presentation as well as the devastating consequence of posterior scleritis. Clinician must maintain a high index of suspicion for posterior scleritis in patients who present with painful blurring of vision. Loss of vision is the most important complication of posterior scleritis and all patients with posterior scleritis must be assumed to be at risk of visual loss. Effort should be made to rule out any systemic association which must be treated promptly.
Correspondence to
Dr. Tan Aik Kah, Trainee Lecturer, Ophthalmology unit, Faculty of Medicine and Health Sciences, University Malaysia Sarawak, Lot 77, Sekysen 22 Kuching Town Land District, Jalan Tun Ahmad Zaidi Adruce, 93150 Kuching, Sarawak, Malaysia. Tel +6082 416550, Fax + 6082 422564, Email: portwinestain@hotmail.com aktan@fmhs.unimas.my