Upper Airway Disease Presenting as Refractory Asthma
B Vahid, J Zangrilli
Keywords
tracheal stenosis, tracheal web, upper airway obstruction
Citation
B Vahid, J Zangrilli. Upper Airway Disease Presenting as Refractory Asthma. The Internet Journal of Otorhinolaryngology. 2005 Volume 4 Number 2.
Abstract
We present a case of tracheal web masquerading as refractory asthma. Flow-volume loop was consistent with fixed airway obstruction. CT scan of neck and bronchoscopy revealed the tracheal web. The patient was treated with tracheal dilatation and tracheostomy.
Case Report
A 62 year old Caucasian female presented to pulmonary clinic with increasing dyspnea on exertion over past year. She reports intermittent wheezing, mild cough, and occasional nocturnal symptoms. She was diagnosed with asthma at another institution and treated with inhaled bronchodilator and corticosteroid treatment with no subjective response. The patient was referred to pulmonary clinic for evaluation and treatment of refractory asthma. Physical examination revealed normal vital signs and oxygen saturation of 96% on room air. Lung auscultation revealed mild bilateral wheezing. Cardiac, abdominal, and neurological examinations were unremarkable. She was a nonsmoker. The patient was treated with Lansoprazole for gastroesophageal reflux disease and had total abdominal hysterectomy done 13 years ago. A chest radiograph and echocardiogram were normal. Pulmonary function testing and flow-loop (Figure1) are shown below.
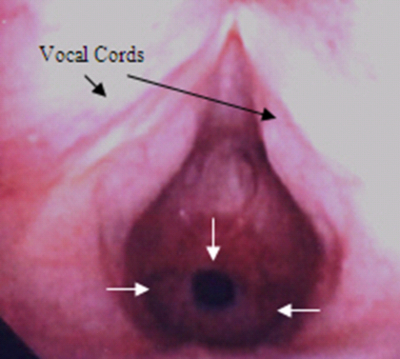
The flow-loop is consistent with fixed airway obstruction. Computed tomography (CT) scan of neck revealed a web-like lesion just below the vocal cords (figure2, arrow) and subsequent bronchoscopy confirmed a membranous subglottic stenosis (figure3, white arrows). The patient underwent tracheostomy and tracheal dilatation.
Discussion
Tracheal stenosis can be congenital or acquired. Congenital tracheal stenoses include fibrous strictures, webs, cartilaginous deformities, and stenoses associated with vascular rings 1. Congenital double aortic arch anomaly masquerading as asthma for thirty years has been described 2. The most common causes of acquired tracheal stenosis are secondary to tracheal injury following a prolonged intubation 3, other traumatic injuries (surgery, blunt trauma), and inhalational injuries 4. Damage to subglottic mucosa due to endotracheal tube may result in ulceration, formation of granulation tissue and subsequently fibrosis and stenosis 3. Incidence of laryngotracheal stenosis secondary to intubation ranges from 1% to 20% in different series 3. Tracheal tumors including tracheal hamartoma 5, neurilemmoma 6,tracheal lipoma 7, glomus tumor of trachea 8, and primary tracheal papillomatosis 9can also present with upper airway obstruction mimicking bronchial asthma. Systemic diseases like amyloidosis and relapsing polychondritis with trachobronchial involvement are rare conditions that may present with wheezing masquerading as bronchial asthma 10, 11. Tracheobronchopathia osteochondroplastica is a rare disease with incidence of 0.002-0.003% in autopsy series. This condition is characterized by presence of bone or cartilage in the mucosa of trachea and bronchi causing an irregular narrowing of trachea or central bronchi 12.
Idiopathic laryngotracheal stenosis (ILTS) is a rare inflammatory disease that results in stenosis of upper trachea. This condition occurs almost exclusively in women. Patients present with dyspnea and stridor 13.
The clinical presentation of tracheal obstruction depends on the degree of lumen reduction and growth rate of the stenosis. Chronic upper airway obstruction can have an insidious presentation. Dyspnea without hypoxemia or hypercapnia is the usual presenting symptom. Patients with 50% to 60% reduction in tracheal lumen present with persistent cough, progressive dyspnea on excretion, and recurrent pneumonias. As the degree of stenosis increases, resting dyspnea and stridor may be detected. Patients with tracheal stenosis are commonly misdiagnosed with asthma or chronic obstructive lung disease. When tracheal stenosis is severe (airway diameter less than 5 mm), alveolar hypoventilation and exertional hypoxemia can be seen 1, 3, 11.
Miller and Hyatt described the physiologic characteristics of obstructing lesions of the larynx and trachea. They found that maximum volunteer ventilation (MVV) and peak expiratory flow rate (PEFR) are the most sensitive measurements to detect mild to moderate upper airway obstruction and forced expiratory volume in 1 second (FEV1) is the least sensitive. They also demonstrated that contour of the flow-volume loop becomes abnormal earlier than other spirometric measurements 14. Fixed airway obstructions produce constant degree of airflow limitation during inspiration and expiration resulting in flattening of both the inspiratory and expiratory portion of the flow-volume loop 11. Helical CT scan of neck with multiplanar reconstructions is 91% accurate in detecting central airway stenosis. Thin-section axial CT scan and conventional tomography also can be used for diagnosis of tracheal stenosis. Direct visualization of central airways with bronchoscopy can confirm the diagnosis 15.
Rigid bronchoscopy with Nd: YAG laser, electrocautery, cryotherapy, mechanical dilation, and stent placement are different interventional modalities useful in management of patients with tracheal stenosis. Tracheostomy and tracheal reconstructive surgery are also indicated in selected patients 3.
Correspondence to
Bobbak Vahid, MD Thomas Jefferson University 1015 Chestnut Street, Suite M-100 Philadelphia, PA 19107 Tel: 215 955-6591 Fax: 215 955-0830 Bobbak.vahid@mail.tju.edu