Addressing Psychiatric Problems of Dementiain the Emergency Room
C Bejjani, G Rumph, M Kunik
Keywords
assessing decision-making capacity, dementia, elders, emergency medicine
Citation
C Bejjani, G Rumph, M Kunik. Addressing Psychiatric Problems of Dementiain the Emergency Room. The Internet Journal of Emergency Medicine. 2012 Volume 7 Number 2.
Abstract
Introduction
Healthcare delivery and cost have been greatly affected by the increasingprevalence of older adults [1]. Currently, older adults account for 12-24% of all emergency room (ER) visits [2], and this will increase over the next decade [1]. In a synthesis of the literature, Grief concluded that ER personnel have limited geriatric training [3];and most report being uncomfortable when dealing with older adults, particularly those with cognitive and psychological problems [2-4].
Approximately 30% to 40% of geriatric patients presenting to the ER have impaired mental status [5-7].Although cognitive impairment is associated with repeatER visits [8], it is rarely addressed in this setting [9].
Identification and Characteristics of Dementia Patients
Persons with dementia have more medical problems than age-matched controls without dementia. This might be explained in part by decreased compliance with medication and discharge instructions [5]. They are also at higher risk for fractures, urgent medical conditions and hospitalization and use psychotropic medications about 9 times more frequently than controls [4]. In addition, approximately 5% of elderly patients present to the ER for psychiatric reasons [10]. Psychosis, agitation, suicidality, depression and substance abuse are frequently the reasons for ER visits by individuals 65 and above [11];however, dementia remains the most common diagnosis. Dementia does not increase the risk of admission to inpatient units unless it is associated with a comorbid psychiatric diagnosis [12].
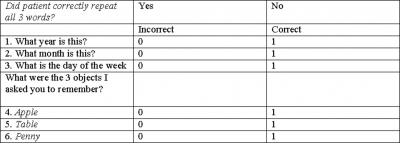
The Geriatric Emergency Medicine Task Force recommends an assessment of mental status for all older patients in the ER [13]. However, a complete diagnosis of dementia and cognitive impairments in the ER is not practical [2]. To address this problem, a 6-item screening questionnaire is useful in the ER to detect patients with cognitive impairment. A score of 4 or less indicates a positive screen for cognitive impairment. It is brief, reliable and comparable to a full Mini Mental State Exam, with a sensitivity and specificity of 88.7 and 88.0, respectively, for the diagnosis of dementia [14](Appendix 1).
Appendix 1
6-Item Screener
1. I would like to ask you some questions that ask you to use your memory. I am going to name 3 objects. Please wait until I say all 3 words; then repeat them. Remember what they are because I am going to ask you to name them again in a few minutes. Please repeat these words for me: APPLE—TABLE—PENNY.
(Interviewer may repeat names 3 times if necessary but repetition not scored.)
Used with the permission of Wolters Kluwer/Lippincott Williams & Wilkins (permission fee to be paid upon acceptance of manuscript).
It is important to differentiate delirium from dementia. Delirium is a state of disturbed consciousness with decreased ability to focus, sustain and shift attention, associated with changes in perception and cognition, which develops quickly and usually fluctuates over the course of a day [15].It is caused most commonly by infections or medication side-effects. Infections, offending medications, dehydration, poor nutrition, stroke, and recent falls/head injury should all be ruled out promptly. Delirium can be very challenging to differentiate from dementia,especially as 50% of delirious patients have underlying dementia [2]. Studies find delirium is diagnosed with high specificity (98-100%) but a rather low sensitivity, ranging from 16-46% [2,16]. An acute onset of confusion is clinically the best way to differentiate delirium from dementia, which, characteristically, has a slower progressive onset. The Confusion Assessment Method (CAM) is a delirium screening questionnaire that can be administered in 5 minutes. It has a high sensitivity and specificity, has been validated in the acute setting and is useful in diagnosing delirium in the ER [17].
How To Communicate With Patients With dementia
ERs are overstimulating, and clinicians should try to interview dementia patients in a calmer, quieter spot without background noise, such as radio or TV. Providers should introduce themselves by name and call the patient by name. It is preferable to speak slowly and clearly and use familiar words and short sentences [18]. The clinician’s demeanor during interviews should be relaxed and not show frustration;meanwhile, he/she should use slow hand gestures, maintain eye contact and provide reassurance and emotional support. Asking simple yes-no questions, limiting choices, repeating key points and nodding in agreement, as well as reframing and rephrasing, are interviewing techniques that are useful in preventing and minimizing frustration. When a patient is upset about a specific topic, one can use distraction (offer a walk, drink or food) and redirection to help him/her focus on a different subject. It is important to remember that patients with dementia cannot always communicate effectively, and it is the provider’srole to make them comfortable and to reorient them to their location and situation.
Providers should avoid using the word
Obtaining Information From Caregivers, Nursing-Home Staff
When assessing a patient with dementia, obtaining reliable information solely from the patient might be very challenging, as patients might have limited insight into their conditionand confabulate or try to hide their disability. It is crucial to get in touch with an informant who can provide accurate information about the patient’s condition, the progression of the disease, precipitating factors and safety concerns that the patient might not be aware of [20]. One should also pay attention to the fact that caregivers can be protective of patients and provide only part of the information. It might be useful in those cases to interview informants separately.
Aggression
Prevalence and Consequences
In persons with dementia, agitation may manifest in a variety of behaviors, including verbal aggression (e.g., yelling), physical aggression, combativeness or resistance to care, psychomotor hyperactivity, and disinhibition. Up to 40% of patients with dementia become aggressive in 1 year [21]. The prevalence of agitation/aggression increases with dementia severity and in institutionalized patients, but there are no differences in the prevalence or phenomenology of agitation across types of dementia [22-24].
In a recently published study, Kunik et al. found that development of aggressive behavior was associated with a 10-fold increase in physical injury [25]. When aggression results in injuries to other residents or staff, a nursing home is likely to send the patient with dementia to an ER. Aggressive behavior is associated with increased use of psychotropic medications and higher rates of nursing-home placements and can also target other nursing-home residents, leading to injuries and frequent police calls, with potential legal consequences for patients and institutions [26]. Physical and emotional aggression towards caregivers can be demoralizing and contributes to higher caregiver burden, which can, in turn, lead to patient neglect and abuse [27].The resulting physical and emotional exhaustion is a common reason causing caregivers to bring patients to the ER [28].
Principles in Addressing Aggression
In the ER, efficiency is critical; and it is useful for ER personnel to have a systematic approach for the differential diagnosis of aggression. Aggression can be secondary to patient, caregiver or environmental factors [19].
Pain is highly correlated with aggression, and one should always screen for it. Several assessment tools have been developed to target the special needs of patients with dementia. The Iowa Pain Thermometer is a validated self-report tool that allows the patient to indicate the degree of pain by marking on a thermometer graphic with verbal descriptors of pain intensity. In addition, because older adults often deny experiencing pain, physicians may consider asking the patient whether he or she experiences “aching” or “hurting “instead of “pain.” In some cases, providers must rely more on observation-based assessments for cognitively impaired patients who cannot verbalize pain [27]. The Non-Communicative Patient’s Pain Assessment Instrument is an example of a valid observational scale appropriate for use with dementia patients [29].It is a brief measure that can be easily administered. Positive screens should be followed by careful, comprehensive physical and psychosocial evaluation to detect causes for the pain [27].
Changes in medication (e.g., anticholinergic side-effects) and the patient’s medical condition should be considered. Caregivers can be very helpful in providing this information and, if they are not present in the ER, one should make an effort to get in touch with them. Further evaluation includes a thorough physical examand baseline lab work to rule out any occult medical problem, such as infections, constipation, urinary retention or fractures. The possibility of substance use (illicit drugs or alcohol) should not be overlooked [19].
Caregiver burden and the relationship of the caregiver with the patient should be assessed in the ER, as they are predictive factors for aggression. One-on-one interviews and asking simple questions, such as, “Describe your relationship,” or “How are you able to care for him/her?” allow caregivers to be truthful about problems. If social workers or mental health professionals are available, they can assist with such evaluations.
ER providers should use the opportunity to give caregivers appropriate resources. Organizations such as the Alzheimer’s Association (http://www.alz.org) and the Alzheimer’s Disease Education and Referral Center (http://www.nia.nih.gov/Alzheimers), as well as the website of the American Psychological Association (http://www.apa.org/topics/alzheimers/index.aspx), provide valuable information about local resources and offer caregiver-support services, hot-lines, and educational information [27].
Several factors can account for agitation, which is often not differentiated from aggression in dementia patients. For instance, psychosis is associated with agitation in patients with dementia; andappropriate referrals and eventual treatment will have a positive impact on those behaviors.Some environmental factors at the residence of the patient can predispose for agitation. In the ER it is important to ask questions regarding the physical aspect of the house or the facility where the patient resides(i.e., lighting, noise), social interaction and stimulation of the patient, use of restraints and traffic flow, as well as a change of environment, because addressing these factors can result in decreased agitation [30].
Treating the Aggressive Patient in the ER
Because of effectiveness and safety concerns of medication use, especially antipsychotics, there is a need to emphasize nonpharmacological interventions in treating behavioral disturbances [31].
ER personnel should be trained to recognize early signs of violence, such as threats; expressing a fear of losing control; a tense, rigid posture and startling easily. Also, when behavior alternates between cooperation and belligerence, it might be an early indication of potential aggression. Clinicians should also trust their feelings when patients make them anxious or fearful.
When facing a potentially aggressive patient, the “least restrictive method of restraint” should be used. Providers need to try to avoid escalating the situation and give the patient the opportunity to cooperate. Fostering a good therapeutic alliance is key to de-escalating a violent behavior and can be sometimes achieved by reassuring the patient, adopting a passive posture and avoiding challenging and provocative remarks. In some instances, telling the patient directly that he/she is scary might help calm him/her. When these approaches fail, try to enlist a friend or a family member’s help to de-escalate the situation.
When the behavior cannot be de-escalated, the use of restraints becomes necessary to protect the patient, staff or a third party. Here too, first give the patient the opportunity to participate in his treatment; as he/she might prefer 1 method of restraint over another.In cases when it is not possible to engage the patient, the ER physician should gather a team, including 4-5 security officers, who would stand 10-15 feet away from the patient and inform him/her in a firm, nonthreatening voice that restraints will be used unless he/she cooperates immediately.
Restraints include seclusion and physical or chemical restraints. Seclusion is the least restrictive method of restraint and should be used first when available in an ER.When appropriate seclusion rooms are not available or a patient does not respond to seclusion, physical and/or chemical restraints should be used. There is evidence that restraints may increase therisk of falls and contribute to cognitive decline [32],and it is up to the clinician‘s judgment to determine the urgency of the situation.
If the patient is willing to take his/her medications beforethe use of physical restraints, this might increase cooperation with physical restraints. If not, physical restraints should be applied as part of a team effort, with assigned functions to each member, while emphasizing the therapeutic and nonpunitive aspect of the procedure. Most often the 4 limbs are restrained, and it is important to keep patients in an open area where they can be monitored with frequent changes of position and regular checks of the neurovascular function of the restrained limbs. This is of utmost importance in a demented patient who is likely to have several medical problems.
Documentation is crucial in this regard, as it is the physician’s responsibility to ensure that the restraints are not negligently performed. Each state and hospital has a specific set of laws and regulations with which ER physicians should become familiar. Four important elements should be documented, in general: (1) the reason for restraints (potential to harm self or others),(2) the measures taken to avoid restraints (talking the patient down),(3) the type of restraints being used and why and(4) the plan to remove restraints when the patient exhibits self restraint.
At times, chemical restraints are necessary, even after the use of physical restraints if the violent behavior continues. In this case, providers should attempt to gather as much information as possible prior to administering the medications; as they might alter the patient’s behavior, rendering the diagnosis more difficult. The oral form is always preferred when possible, but at times the use of an intramuscular form is necessary when the patient is unwilling to cooperate. In the elderly, and especially in those with dementia, the choice of medications used should be carefully considered; as these patients are especially sensitive to side-effects. Despite the well-established risk of pharmacotherapy in this population, when behavioral measures alone are insufficient, the American Psychiatric Association (APA) guidelines support the use of antipsychotic medications [32].Haloperidol, a typical high-potency antipsychotic, is effective for controlling acute agitation, especially when psychotic features are present [33]. Advantages include its availability in oral, intramuscular and intravenous forms; but one should be cautious, given the higher risk of extrapyramidal side-effects [33]. The newer atypical agents, such as olanzapine, quetiapine, risperidone, and ziprasidone, have fewer extrapyramidal side-effects and may be particularly useful in patients with Parkinson’s disease [33].However, quetiapine is not used when an abrupt change in behavior is needed, as it carries recommendations for slow titration.Risperadal comes in both a liquid and a dissolvable-tablet form, which is helpful when cheeking and noncompliance are suspected. Olanzapine and ziprazidone come in oral and IM forms,useful for agitated patients who refuse oral medications. Studies failed to show evidence that 1antipsychotic is more effective than others, so the choice should be guided by the side-effect profile that could benefit or harm each particular patient [32].
Benzodiazepines can be used alone or in conjunction with antipsychotics to treat acute agitation in patients with dementia, especially in patients in whom anxiety is prominent. Lorazepam is preferred because it does not have an active metabolite and does not require oxidative metabolism in the liver.It can be given either orally or intramuscularly on an as-needed basis in doses from 0.5 to 1 mg every 4 to 6 hours,with a maximumof 1–3 mg of lorazepam (or equivalent doses of otherbenzodiazepines) in 24 hours.Frequent side-effects includedisinhibition,confusion, oversedation, falls, and delirium; so providers should use them with caution and after excluding potential contraindications in the individual patient [32].
Psychosis
Prevalence and Consequences
Up to 41.1% of patients with AD experience psychotic symptoms at some point over the course of their disease [34]
Several studies have linked psychotic symptoms in dementia to increased aggression and agitation. This is likely to lead to increased caregiver burden, emotional distress in patients and more ER visits [35,36].
Principles in Addressing Psychosis
Patients presenting to the ER with psychotic symptoms should first undergo a thorough medical and neurological evaluation to rule out a possible underlying medical illness or drug toxicity that could be easily reversible [37]. Specific attention should be geared towards delirium, as many psychotic symptoms occur in that context.Providers should then assess the psychiatric status of the patient to rule out a previous psychiatric diagnosis such as schizophrenia. Collateral information provided by caregivers is valuable in this instance. Once all other causes of psychosis are ruled out, the patient is considered to have psychosis of AD.
The APArecommends treating psychotic symptoms with nonpharmacological measures when they are not associated with agitation and/or aggression and when they do not cause significant distress to the patient.Behavioral strategies can include environmental changes and effective communication techniques [38].
The APA supports the addition of low doses of antipsychotic medications when severe distress occurs and/or there is concern about the safety of patients or caregivers [32]. A great deal of caution is indicated when starting these medications. In April 2005, the US Food and Drug Administration issued a black-box warning about increased risk of death and cerebrovascular events in elderly patients with dementia who are taking conventional or atypical antipsychotics. The American Association of Geriatric Psychiatry issued a letter to healthcare professionalsstateing that the black-box warning should not preclude professionals from prescribing antipsychotics when needed, as they have been proven to be efficacious in treating behavioral aspects of dementia. However, it strongly emphasized the importance of discussing potential side-effects, including increased mortality and cerebrovascular events, with patients and caregivers and including an informed consent in the chart [39].
Among the atypical antipsychotics, no agent has been approved by the FDA for the treatment of psychosis in dementia [40], but a Cochrane Collaboration review of placebo-controlled trials concluded that risperidone and olanzapine may improve aggression more than placebo and that risperidone may improve psychosis relative to placebo [41].
Wandering
Prevalenceand Consequences
Wandering occurs in up to 65% of nursing facility residents and dementia clinic patients and in 36% of community-dwelling patients [42]. Although there is no universal definition of the term, the most-used definition of
Wandering becomesa concern when it takes the place of a meal and/or causes fatigue, exhaustion or physical injury [38,44]. It can also be bothersome when the wanderer is rummaging, touching others, eating others’ food or entering other people’s rooms [38].
Critical wandering occurs when patients cannot be located or when they wander away from a controlled environment and supervised care [45]. This has been associated with physical harm, emotional distress, earlier institutionalization and death [46]. It can also cause the caregiver feelings of guilt and fear of reprisal and institutions to implement more restrictions, as well as potential lawsuits [38].
When supervised, wandering can provide an individual with an opportunity for physical activity, improved circulation and oxygenation and decreased contractures. Pacing, in particular, has been shown to be an indicator of good health, as evidenced by good appetite, less pain, fewer diagnoses and fewer medications than in those with dementia who do not wander [44].
Principles in Addressing Wandering
In the ER the main concern should be to rule out any potential complication that might have resulted from wandering, including physical injury, dehydration, fractures, metabolic imbalance, fatigue, failure to have taken necessary medications while wandering or signs of abuse. It is also important to assess and treat underlying causes that might have precipitated the behavior or led to confusion, such as anxiety, spatial disorientation, delusions or hallucinations [38]. A social-work consult can assist in getting in touch with the caregivers or institution where the patient resides if she/he is unable to provide such information. The ER could also be a place to educate caregivers about resources that help with early intervention programs, such as the Alzheimer’s Association Safe Return program and the MedicAlert program [38].
Physical barriers and physical restraints have been used traditionally to prevent wandering. Pharmacotherapy with neuroleptic drugs has undesirable side-effects and has shown only modest efficacy [46]. In the ER, patients should be placed far from exit signs/doors. Staff/family members should walk with them when they going to the restroom or a different location if a test is needed, for example. Subjective barriers,such as mirrors, camouflage, and grids/stripes of tape, can be used. Electronic locks or electronic devices that trigger an alarm when the patient tries to leave could be helpful. The addition of a more complex or less accessible door latch might make it harder to wander away from the ER than usual [32].
Resistiveness to Care
Prevalence and Consequences
Patients who refuse care may present to the ER because their refusal has led to medical problems or aggression/staff assault. Medical problems may result from their refusal to take medications or refusal to eat or drink. Resistiveness to care (RTC) is defined by the behaviors used by persons with dementia to oppose care. It usually occurs when caregivers are delivering hands-on care or trying to redirect the patient[38,47] and may lead to aggression and assault of both patients and staff. Patients resist when they believe that care is not needed or when they do not understand the motives behind the caregiver’s actions [47]. Physical injury of family members or long-term-care staff will often result in an ER visit.After analyzing data of 23,837 nursing-home residents with Alzheimer’s disease,Volicer et al. found that RTC alone was present in 9% of residents; whereas it was accompanied by agitation in 8% [47].
Principles in Addressing Resistiveness to Care
ER staff need to assess for any medical or metabolic complications that might have resulted from refusal of fluids, nutrition or medications or that might have precipitated a delirium causing RTC.
Psychosis is another comorbidity that should be screened for when faced with RTC.For example, a delusional patient might think that food or medications are poisoned and therefore refuse them.When a patient declines the offered procedure, distraction (when 2 providers are available) or delaying care(if medically possible) prevents escalating behaviors. Other strategies include modification of a nursing procedure to match a patient’s preference. Trying to make personal space more personal(curtains), adjusting lights to avoid a glare, decreasing noise, asking 1 question at a time, adjusting the room temperature or using blankets to keep patients warm might decrease anxiety and encourage patients to consent to procedures [38].RTC will be encountered more frequently in the future, and it will be beneficial to have ER personnel (nurses or technicians) trained in some useful but morelengthy approaches. The
Medical professionals should be very careful to balance the advantages and burdens of each medical procedure, even simple ones, such as blood drawing, as individuals with dementia might not always understand the rationale behind them, leading to RTC. It is recommended that clinicians have clearly defined goals of care in managing medical problems [38].
Capacity
Patients with dementia are more likely to have impaired decision-making capacity and decisional abilities than older adults without dementia [48,49]. This, however, does not mean that the diagnosis of dementia alone is sufficient to confer decisional incapacity on patients. In ERs, providers often have limited time to establish capacity for complex situations. Capacity is often implicitly established during history taking and the physical exam of a lucid patient. Questioning about orientation or asking the patient to communicate his/her understanding of the situation and of the procedures/alternatives isoften sufficient to allow classification of them into 4 categories: “able to interact meaningfully,” “able to interact on a limited basis,” “unable to interact meaningfully,” or “essentially vegetative.” When patients are in the last 2 categories, they are deemed to be without capacity. Other tools can be used to help guide this decision, such as the 6-item screening questionnaire, the clock-drawing test and the orientation memory concentration test [50].
Some patients have executed a legal document identifying a surrogate or specific instructions (living will, advanced directive) that must be honored. In other cases, providers must seek consent from the next of kin, as determined by their state laws. When care is truly urgent, implied consent is acceptable; and the ER physician must proceed with the treatment of a patient with impaired capacity. However, when a clinician knows that a patient with impaired capacity will refuse treatment, he/she should not wait until an emergency exists to proceed without consent [51].
Neglect/Abuse
Neglect and abusecan be physical or psychological and harm a patient with dementia by mistreatment and/or lack of attention and care. Identified risk factors for neglect or abuse can be related to the caregiver, patient, relationship or environment [52].Cognitive impairment may limit patients' ability to report abuse, and ER providers should screen for potential abuse. Wiglesworth et al. suggested a brief, 6-item screening questionnaire for neglect and abuse of people with dementia, which involved the following questions for caregivers: The patient (1) threw something at me that could hurt; (2) pushed or shoved me; (3) grabbed me; (4) insulted or swore at me; (5) shouted or yelled at me; or (6) stomped out of the room, house, or yard during a disagreement [52].
When mistreatment is suspected, providers should rule out immediate danger. In case of immediate danger, a safety plan is elaborated; and it could include hospital admission(only if a patient who has capacity consents), a court order or safe home placement. If no immediate danger is identified, a full private assessment should be performed, either in the ER if the structure allows it or scheduled for later [53]. Referral to social services when available is valuable, as it will provide the patient with appropriate resources and help with relocation as needed [52].
Working With Multiple Disciplines in Assessment and Intervention
An integrated, interdisciplinary approach improves dementia care and health-related quality of life [54]. It is outside the scope of the ER setting to address all complex components of dementia; but, based on the urgency and the nature of the patient’s presentation, immediate consultations or delayed referrals can be very helpful. In case of placement problems; difficulty reaching a reliable informant; or the need for referrals to social, legal, home health and financial services, a social-work consult can be very helpful. In cases where there is no previous diagnosis of dementia or in cases in which a previously diagnosed patient has no regular follow-up, ER providers should refer to primary care follow-up or to a cognitive clinic, depending on the institution’s regulations, only after confirming that the patient is in a safe environment, has caregivers and is otherwise safe.
Conclusion
The practice of emergency medicine is challenged to provide care to a growing body of elderly Americans; and, with an expectation that 11 to 16 million people will be diagnosed with dementia in 2050, it is important to begin changing practice habits now. Incorporating the above screening items, calm environments, management techniques, and additional training for nurses and care technicians are essential. Additionally, using the correct means of restraint (verbal, physical, or chemical) can promote shorter visits and less delirium and injury. Learning and using the necessary skills to establish likely capacity and preserve self esteemfor these patients also promote better care and outcomes.
Acknowledgments
This work was partly supported by the resources and facilities of the VA HSR&D Houston Center of Excellence (HFP90-020). The views expressed are those of the authors and not necessarily those of the Department of Veterans Affairs/Baylor College of Medicine.