Gastric Lipoma Presenting As Gastrointestinal Bleeding: A Case Report
A Ciraldo, D Thomas, S Schmidt
Keywords
gastric lipoma, gastrointestinal bleeding, medicine, oncology
Citation
A Ciraldo, D Thomas, S Schmidt. Gastric Lipoma Presenting As Gastrointestinal Bleeding: A Case Report. The Internet Journal of Emergency and Intensive Care Medicine. 1999 Volume 4 Number 2.
Abstract
Gastrointestinal lipomas are benign tumors of the gastrointestinal tract, constituting only 5% to 6% of all gastrointestinal tumors (1,2,3). The majority (60-75%) of gastrointestinal lipomas are located in the colon (1,4), followed by the small intestine (20-25%) (4). Gastric and duodenal lipomas are extremely rare. Gastric lipomas account for only 3% of all benign neoplasms and 5% of all gastrointestinal lipomas (5,6). Due to the rarity of the lesion, gastric lipoma is often difficult to diagnose. It may mimic peptic ulcer disease, gastric outlet obstruction, or present as acute upper gastrointestinal bleeding. We present one such case of gastric lipoma that presented as an acute upper GI bleed.
Reprint requests and correspondence may be addressed to:
Steven Schmidt, PhD
Summa Health System
Division of Surgical Research
525 East Market Street
Akron, Ohio 44314
Phone (330) 375-3693
Fax (330) 375-4648
schmidts@summa-health.org
Case Report
The patient was a 65-year-old white male who presented to the emergency department with the chief complaint of black tarry stools and light-headedness of two days duration. He denied any nausea, vomiting, reflux symptoms, hematemesis, or abdominal pain. He stated that his bowel movements were usually formed and occurred once to twice per day. He denied alcohol use but did note that he took one aspirin per day. He did have a smoking history of 1.5 packs of cigarettes per day for 40 years, but quit ten years ago. His past medical history was significant for hypertension, gout, hypercholesterolemia, coronary artery disease CAD, and history of a myocardial infarction two years prior treated with coronary angioplasty. His medications included: aspirin, Zocor, allopurinol, Zestril, Cardizem, Demadex, Indocin, and Claritin.
During physical exam no abdominal pain was elicited nor were any abdominal masses palpated. Stool was guaic positive. An NG tube was placed in the emergency department and the aspirate was positive for clotted blood.
Initial laboratory studies revealed: WBC 9.7; hemoglobin 12.3; hematocrit 36.8; platelets 235. Blood chemistry profile and coagulation studies were within normal limits.
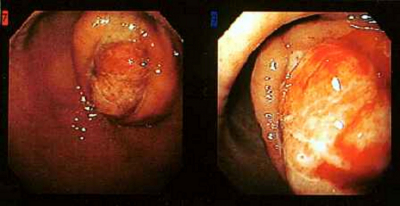
The patient was then referred to a gastroenterologist for esophagogastroduodenoscopy (EGD). EGD revealed an approximately 3 cm in diameter gastric polyp that was located at the junction of the antrum and body of the stomach (figure 1). Gastric mucosa enclosed the polyp, creating the illusion of an approximately 5 cm in diameter polyp. An area of ulceration was present at the edge of the normal mucosa. No visible vessels were seen and no bleeding could be elicited from the ulcerative area. The esophagus and duodenum were normal. Multiple biopsies were obtained.
Figure 1
At this time, surgical consultation was obtained as well as a CT scan of the abdomen.
The CT scan revealed a low attenuation rounded fairly well defined soft tissue mass in the gastric antrum, measuring approximately 3 x 3.5 cm in diameter (figure 2). The presence of a gallstone was also noted. The mass was suspected to be a leiomyoma or leiomyosarcoma.
The patient was scheduled for resection of the gastric mass and cholecystectomy. In the interim period before surgery his hemoglobin and hematocrit decreased to 10.4 and 31.4, respectively. At laparotomy, no other masses were found in the abdomen except for a very soft, rounded mass in the gastric antrum. The stomach was opened on the greater curvature and an ulceratous lesion was located overlying the mass. The mass was located between the serosa and submucosa. Upon inspection, it was evident that the overlying mucosa had broken down and ulcerated into the mass. The mass was then excised with clear margins. The excised mass felt soft and rubbery, much like a benign lipoma. A frozen section was obtained by pathology and the results indicated that the tissue was a lipoma with reactive and inflammatory changes. The abdomen was again inspected for signs of metastasis, which were not found. The stomach was then closed and the omentum was sewn over the closure. Next, a cholecystectomy was performed, hemostasis was obtained, and the abdomen was irrigated and closed without incident.
Final pathological diagnosis determined the mass to be a submucosal lipoma with associated fat necrosis and acute and chronic inflammation and ulceration of the overlying mucosa. The gallbladder specimen revealed cholelithiasis with associated chronic cholecystitis.
Figure 3
The patient underwent an uneventful recovery and is doing well today. Two years have since passed since his surgery and no further bleeding or evidence of lipoma recurrence has been detected.
Discussion
The discovery of a gastric tumor carries a worrisome prognosis. 75% of all tumors located in the stomach are carcinomas (7), whereas 15% of gastric tumors are benign (7), making it imperative to obtain a histologic diagnosis. Several useful endoscopic findings have been reported to be positive predictors for the presence of a benign gastric lesion. These include: a sharply defined, soft submucosal mass, often yellow in color as opposed to the surrounding pink mucosa, which may be associated with a centrally located superficial ulceration caused by pressure necrosis; the presence of the “bridging folds” sign, in which the surrounding gastric mucosa is visualized to be pulled up to and surrounding the edges of the tumor; the “tenting sign”, in which the overlying mucosa is easily retracted with the biopsy forceps; and the “cushing sign”, in which an impression remains in the mass after compression by the biopsy forceps (1,5,8).
The etiology of gastric lipomas is unknown (8) and the incidence is equal in both sexes (2,8). 75% of gastric lipomas are located in the antrum and are usually submucosal in origin (1,2,8,9). Less than 5% are subserosal in location (4,9). Gastric lipomas are usually asymptomatic (4,9) and tumor size usually dictates occurrence of symptoms. Tumors less than 1 cm in diameter are usually asymptomatic, whereas 75% of lesions greater than 4 cm in diameter become symptomatic (4). The most common presenting symptom is gastrointestinal bleeding, occurring in over 50% of patients (2,8,10,11). Other presenting symptoms may include hematemesis, obstruction, vomiting, and dyspepsia (2,12).
Gastric lipomas have never been shown to have potential for malignant transformation (1,2,5,9). The treatment of choice for a symptomatic gastric lipoma is circumferential excision with a clear margin of normal tissue (2). Incisional biopsy may be performed for very large tumors. Histological diagnosis is essential in either case to rule out malignant lesions. Upon return of the histological diagnosis of lipoma, the tumor should then be excised and shelled out (2). Due to the benign nature of this lesion an extensive surgical procedure such as an extended gastrectomy is not necessary. Simple local enucleation or partial gastric resection is sufficient to remove the lipoma without fear of relapses or malignant degeneration (1). In our patient, surgical excision was necessary for definitive diagnosis and treatment of his bleeding ulceratous lesion.