Folliculotropic Mycosis Fungoides: Response to Bexarotene
R Talpur, M Duvic
Citation
R Talpur, M Duvic. Folliculotropic Mycosis Fungoides: Response to Bexarotene. The Internet Journal of Dermatology. 2008 Volume 7 Number 3.
Abstract
Folliculotropic mycosis fungoides (FMF) is a variant of mycosis fungoides characterized by the presence of folliculotropic infiltrates, often with sparing of the epidermis, and preferential involvement of the head and neck. We report a man who was initially diagnosed with eosinophilic folliculitis but had classical FMF with ulceration and improved on bexarotene.
Introduction
Folliculotropic mycosis fungoides has been designated as a distinct entity in the World Health Organization-European Organization for Research and Treatment of Cancer classification system for cutaneous lymphomas. 1 It usually involves the scalp and face but may also compromise the torso, as in our patient. Its clinical spectrum includes scarring and non-scarring alopecia, erythematous plaques with follicular accentuation, acneiform lesions such as nodulocystic lesions, pustules, milia and comedones, tumors, and sometimes mucinous discharge. Severe pruritus is also a prominent feature. 2
Initial Presentation
A 62-year-old man presented with a 20 year history of a pruritic erythematous rash on his scalp and trunk that had been diagnosed as seborrheic dermatitis and eosinophilic folliculitis. He had eosinophilia (13%) and IgE significantly elevated (2317 K/UL). He was initially treated with systemic antifungals, topical steroids, antihistaminics and oral antibiotics with partial improvement. This past last year, he developed a slowly growing ulceration in the middle of his back.
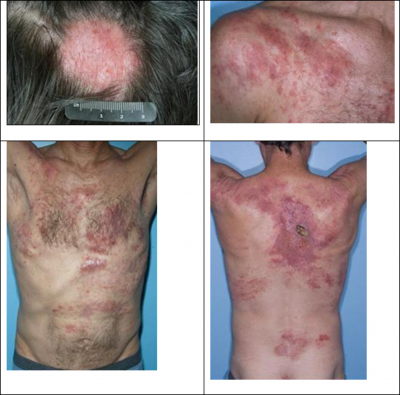
Physical examination (Figure 1A) revealed an erythematous plaque with scarring alopecia on his scalp and (Figure 1B) erythematous telangiectatic patches and plaques on the trunk. Micropustules were seen within some of these lesions. (Figure 1C). On the back, he had a large 4 x 3 cm. ulcer down to the muscle containing purulent drainage (Figure 1D) and had palpable axillary and inguinal nodes. The cultures grew Staphylococcus aureus. Biopsies were performed of the edge of the ulcer, of the anterior chest surrounding a pustule, and of a lymph node.
Figure 1
Diagnosis: The patient was diagnosed with Folliculotropic mycosis fungoides stage IIA (T2N0M0).
Microscopic findings and clinical course
Two sets of biopsies were examined. The initial biopsy (dated 2002) showed a mild perifollicular infiltrate composed of lymphocytes and some eosinophils. A few eosinophils were reported to be present in the epidermis. A diagnosis of eosinophilic folliculitis was made in an outside institution. Subsequent in house biopsies, taken 6 years later, showed a dense lymphocytic infiltrate with prominent folliculotropism. Some epidermotropic cells were also seen. (Figure 2A) The infiltrating lymphocytes displayed mild cytologic atypia (Figure 2B). Plasma cells and eosinophils were also present. Immunohistochemical studies revealed the lymphocytes to be CD3-positive T cells (Figure 2C); rare CD20-positive B cells were identified. The folliculotropic and epidermotropic lymphocytes were mainly CD4 positive (Figure 2D). Scattered CD8-positive cells were seen within the follicles and epidermis (Figure 2E). Diffuse positivity for CD25 by > 75% of the atypical lymphocytes was observed in one of the biopsies. Re-examination of the original biopsy showed a population of atypical, epidermotropic CD3-positive lymphocytes, positive for CD4 and negative for CD8. The epidermotropic and folliculotropic lymphocytes had a CD4:CD8 ratio of about 4:1. A diagnosis of mycosis fungoides, folliculotropic variant, was made on both sets of specimens. Molecular studies for TCR gamma gene rearrangement identified a monoclonal population, supporting the diagnosis of mycosis fungoides. Lymph node biopsy showed follicular hyperplasia.
Figure 2
Treatment Course
The clinical course was consistent with folliculotropic mycosis fungoides, Stage IIB. He was started on oral bexarotene 150 mg, dicloxacillin 500 mg twice daily, and topical mupirocin with considerable improvement of cutaneous lesions (Figure 3). The patient subsequently developed new papules on lower extremities and was started on nitrogen mustard alternating with betamethasone on lesions.
Discussion
Five distinctive histological patterns have been described in FMF which are considered to be highly characteristic. They are 1] intact follicles with folliculotropism with or without mucin, 2] basalloid folliculolymphoid hyperplasia, 3] cystic, 4] granulomatous and 4] eosinophilic folliculitis. Our patient had classic folliculotropcic lesions but with eosinophilia and deep ulceration, which is an unusual presentation. He was misdiagnosed with eosinophilic folliculitis initially rather than FMF. 3
Hypereosinophilia and elevated IgE levels have been reported in mycosis fungoides in the absence of any other underlying cause 4 but are not common in FMF. In advanced stages of CTCL, a shift in cytokine profile from TH1 to TH2 is observed, which coincides with eosinophilia, high levels of immunoglobulin E, and increased susceptibility to bacterial infections. 5 These features might be associated with longstanding FMF but not necessarily with advanced stages.
FMF is more refractory to treatment since the cells are in the dermis, and has a worse prognosis than the classic type of MF. Best results have been reported with psoralen plus UVA (PUVA) therapy with oral bexarotene or PUVA with interferon alfa. 26 However, there is a report of a complete response with low dose (150mg) oral bexarotene monotherapy in a patient with acneiform lesions on her face and back, similar to our patient. 7 Since FMF may present with atypical clinical and histological features, its diagnostic and treatment might be delayed. Cases of FMF that are refractory to retinoids or interferon plus PUVA may require electron beam radiation which is usually effective in treating existing lesions, although the disease may relapse later.