Topical Tacrolimus for the Treatment of Oral Lichen Planus
E Stoopler, T Sollecito, S DeRossi
Keywords
corticosteroids, oral lichen planus, tacrolimus
Citation
E Stoopler, T Sollecito, S DeRossi. Topical Tacrolimus for the Treatment of Oral Lichen Planus. The Internet Journal of Dermatology. 2002 Volume 2 Number 1.
DOI: 10.5580/1528
Abstract
Lichen planus is a chronic inflammatory mucocutaneous disease that can have both cutaneous and oral involvement. Clinical presentations of oral lichen planus are varied and the erosive form can be the most symptomatic and difficult to treat. New research in cytokine biology may begin to help explain the pathogenesis and chronicity of oral lichen planus. Conventional treatment for oral lichen planus includes topical and intralesional corticosteroids. Tacrolimus, a calcineurin-inhibitor, has been shown to be effective in treating lesions of erosive oral lichen planus that are recalcitrant to topical steroid therapy. We would like to present a case in which a patient with severe erosions of the tongue, due to oral lichen planus, was effectively treated with topical tacrolimus following unsuccessful topical and intralesional steroid therapy.
Introduction
Lichen planus is a relatively common dermatologic disorder that occurs on the skin and oral mucous membranes. There are several forms of oral lichen planus (OLP); however, the most common and most readily recognized from is the reticular form, consisting of slightly elevated, fine, whitish lines (Wickham's Striae) that produce a lacelike lesion. Erosive OLP presents as chronic multiple oral mucosal ulcers. Recent studies involving T cells and immunomodulating cytokines, including TNF – alpha, may provide clues as to the pathogenesis and chronic nature of OLP. 1 Patients with reticular OLP frequently are asymptomatic and may not require any treatment. Patients with erosive OLP frequently experience a great deal of discomfort and pain and need to be managed more aggressively. High potency or ultra high potency topical steroids can be used to treat erosive lichen planus and may provide relief to patients. Intralesional steroids can be used for indolent lesions that may not respond to topical steroid therapy. Tacrolimus is a calcineurin-inhibitor initially used to prevent solid organ allograft rejection. Topical formulations of tacrolimus have been developed for use to treat atopic dermatitis. 2 We would like to present a case in which a patient with severe erosions of the tongue, due to OLP, was effectively treated with topical tacrolimus following unsuccessful topical and intralesional steroid therapy.
Case Report
A 56-year-old white female presented to the Oral Medicine Clinic with a chief complaint of sores on her tongue and mouth for the past 13 months. Her symptoms began following an extended trial of antibiotics for sinusitis and bronchitis. A biopsy was performed and confirmed the histopathologic diagnosis of erosive lichen planus.
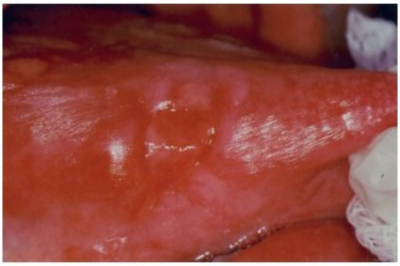
Her past medical history is significant for hypercholesterolemia, bipolar disorder, asthma, and hypothyroidism. Current medications include amoxapine, gabapentin, fluoxetine, fexofenadine, ibuprofen, clonazepam, atorvastatin, methylphenidate, levothyroxine, estrogen, and ipratropium. A comprehensive review of systems was significant for some mild heat intolerance and some numbness of her right arm and pain in her lower back. Clinical examination revealed no cervical lymphadenopathy, salivary gland enlargement or lesions on exposed skin surfaces. She had no conjunctivitis. Her oral mucosa was moist with diffuse areas of erythema and desquamation on the buccal mucosa, bilaterally. The tongue had large ulcerations (> 1cm) on the lateral aspects bilaterally (Figure 1).
Figure 1
There were multiple white – yellow small plaques that could easily be removed on the buccal mucosa, confirmed as candidiasis via Gram stain. Initial treatment consisted of clobetasol gel 0.05% applied to the affected areas 3 times per day and Mycelex troches 4 times per day. Clinical exam at one month revealed 10% resolution in the lesions on the buccal mucosa and lateral border of the tongue. The candidiasis had completely resolved. Treatment with intralesional injections of triamcinolone 5mg / cc combined with topical corticosteroids resulted in an additional 15% improvement in signs and symptoms over the next two months. The patient was placed on topical tacrolimus 0.1% 3 times per day and evaluated at 2 months. Subjectively, she noted 50% improvement of symptoms and on 4 month follow up, noted 75% overall improvement. Clinically, there was 90% improvement in erythema and 100% resolution in ulcerations over the same period (Figure 2). The patient is continuing to use topical tacrolimus 2 times per day, and undergoing 6 month follow up.
Discussion
Lichen planus is a chronic inflammatory mucocutaneous disease affecting 0.5 to 1% of the adult population. 3, 4 Patients can have both cutaneous and oral involvement. 5 Clinical presentations of OLP are varied and are frequently reported as reticulated, plaque – like, erosive, papular, atrophic, and bullous. The reticular form is the most common; however, the erosive, atrophic, and bullous forms are the most symptomatic and most difficult to treat. All regions of the oral cavity may be affected; however, most commonly, lesions are found on the posterior buccal mucosa and, in order of decreasing frequency, the gingiva, tongue, palate, lip, and floor of the mouth. 6
Cell mediated immunity seems to play a critical role in the pathogenesis of lichen planus. Though the specific antigen(s) responsible for the activation of T cells has not been identified, studies have demonstrated the interaction of T cells and mast cells in a cyclical nature via the production of cytokines, such as RANTES (regulated on activation, normal T-cell expressed, and secreted) and TNF alpha, which may explain the chronicity of this disease. 7 Investigations have demonstrated the production of RANTES and the presence of specific RANTES receptors, such as CCR1, on T cells and mast cells in OLP lesions. 1 TNF – alpha, an inflammatory mediator, has been shown to up-regulate expression of CCR1. This suggests that RANTES, CCR1, and TNF – alpha interact and may be involved in the accumulation of inflammatory cells in OLP. 8 Dental amalgam has been shown to increase TNF – alpha concentration in peripheral blood mononuclear cells 9 and may be a causative agent of OLP eruptions. Medications, flavoring agents, and viruses have also been reported to be associated with OLP eruptions. 10
Treatment for OLP includes topical and intralesional high – potency corticosteroids, retinoids, cyclosporine, and most recently, topical tacrolimus. Recent evidence – based reviews showed topical corticosteroids were the most effective treatment. 11 Topically, both 0.1% tretinoin and 0.1% isotretinoin (retinoids) have been used for the plaque – like form of the disease. Topical cyclosporine has not demonstrated superior efficacy compared to topical corticosteroids alone. 12
Tacrolimus, a member of the immunosuppressive macrolide family, suppresses T-cell activation by binding to cytosolic FK – binding proteins, which, in turn, interferes with the calcium / calmodulin – dependent phosphatase calcineurin. 13, 14 This ultimately results in the inhibition of cytokine gene transcription, including Interleukin 2 and TNF – alpha. 15 Topical tacrolimus was shown to be efficacious in atopic and contact dermatitis. 14, 16,17,18 Initial anecdotal evidence reported patients with recalcitrant erosive OLP were treated with topical tacrolimus and either substantial resolution or complete resolution of the lichen planus was noted over a period of time. 19 More recent studies have also demonstrated the efficacy of tacrolimus in treating erosive OLP. 20,21,22 Topical tacrolimus has been shown to produce significantly less skin atrophy than topical corticosteroids. 15 Although tacrolimus ointment is available in 2 strengths, 0.1% and 0.03%, the 0.1% formulation has been shown to be more effective in treating erosive lesions of OLP. 15 The major adverse reaction reported with topical tacrolimus is local irritation at the site of application. 15 Pimecrolimus, a second generation calcineurin – inhibitor, has been developed to treat atopic dermatitis. The major advantage reported when using topical pimecrolimus is significantly less irritation at the site of application in comparison to topical tacrolimus 15 Pimecrolimus is available in a cream vehicle only, making it extremely difficult to use intraorally due to its inability to adhere to moist oral tissues. Therefore, there have been no reports of using pimecrolimus, thus far, to treat erosive OLP.
Conclusion
Topical use of tacrolimus is a safe, well tolerated, and effective therapy for oral lichen planus lesions recalcitrant to traditional therapies. New research in the areas of immunomodulation and cytokine biology may elucidate the molecular milieu attributed to the pathogenesis and chronic nature of OLP.
Correspondence to
Eric T. Stoopler, D.M.D. Department of Oral Medicine University of Pennsylvania School of Dental Medicine 240 S 40th St., Philadelphia, PA 19104 Phone: 215.746.0112 Fax: 215.898.7853 Email: ets@pobox.upenn.edu