New Biomedical Devices And Documentation Of Brain Death
G Litscher
Keywords
acti, anesthesia, anesthesiology, bioelectrical signal recording, brain death, critical care medicine, education, electrodes, electroencephalography eeg, electronic publication, intensive care medicine, internet, isoelectric eeg, multimedia, online, peer-review, regional anesthesia, sonography tcd, transcranial doppler, trauma, ve cable electrode
Citation
G Litscher. New Biomedical Devices And Documentation Of Brain Death. The Internet Journal of Anesthesiology. 1998 Volume 3 Number 4.
Abstract
Conventional techniques to record bioelectrical signals are sensitive to artifacts, particularly in the critical care setting. An active cable electrode was d
eveloped to reduce artifacts with measurements in very small dimensions (< 0.7
µVpp). The new device suppressed artifacts and had very low noise activity comp
ared with conventional EEG recordings in a subject during the development of br
ain death.
Acknowledgment: This work was supported by the Austrian Ministry of Science and Transport (GZ 140.508/4-VII/4/97). The author would like to thank Mr. DI G. Raich, Mrs. cand.-ing. Romy Lehmann for her help in data recording and analysis and Mrs. cand. soc. oec. Petra Petz for mulitmedial documentation and manuscript preparation.
Introduction
Brain death is defined as the irreversible cessation of all brain function. The diagnosis of brain death is based primarily on the neurologic examination. Supplementary tests including EEG recordings, evoked potentials, angiography, and, more recently, transcranial Doppler sonography (TCD) are useful to document the dynamics of cerebral circulatory arrest (1).
EEG is a sensitive technique to evaluate the function of the cerebral cortex. In Europe it is the most widely used electronic test in the evaluation of brain death. But the comparability and accuracy of the EEG can be influenced by technical problems and by different evaluation criteria (2). Some patients show cortical EEG activity even after cessation of brain stem function (3). Other patients meet the clinical criteria of brain death but do not have an isoelectric EEG. Still other patients with an isoelectric EEG and absent brain stem potentials have residual cerebral perfusion documented with angiography (4).
New biomedical technologies can register bioelectric activity in the range of <0.7 µVpp, dimensions in which previously signal components could no longer be registered (5,6). These recordings are possible even in the critical care environment. We present a case that illustrates the difficulties involved in defining an isoelectric EEG and the potential of a new technology.
Methods
Active Cable EEG Electrodes
The role of an EEG electrode is to provide an ideal electric contact between the patient and the EEG apparatus. Figure 1 shows new miniature active electrodes that are integrated in a cable. Miniature amplifiers to directly amplify EEG signals at the site of the recording position can improve data quality. These amplifiers are placed directly into a cable. The active cable electrode has a gain of 100 dB for optimal signal quality and adequate voltage level for further signal processing. These electrodes can record EEG signals from an intact skull at a range of <0.7 µV (peak-to-peak) and stimulus-induced oscillations and evoked potentials at a range of <70 nV (5,6).
Figure 1
The cable electrode has a noise level of less than 0.15 µV rms (root-mean-square) from 0.05 – 70 Hz, a common-mode rejection ratio (CMRR) of 115 dB (50 Hz), an input leakage current of 10 pAtyp , an input impedance of 1014 Ohm and a bandpass of 10 kHz. The cable electrode measures 13 x 18 x 2.5 mm.
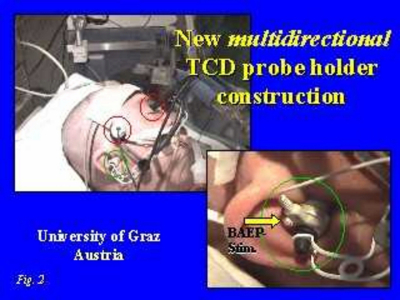
Mulitdirectional Spectacle Frame Holders
We developed a bilateral and multidirectional TCD monitoring arrangement to simultaneously and continuously monitor bloodflow profiles of different extracranial and intracranial vessels (5,7,8) (Fig. 2). The TCD measurements in this study were performed by an experienced investigator with the Multi-Dop-T (DWL-Electronic Systems, Sipplingen, Germany).
Figure 2
Case Report
A 46-year-old-male with a severe head injury was monitored continuously by clinical findings, electrophysiologic tests (EEG, BAEP), and multichannel-TCD. After admission to the intensive care unit, the clinical status deteriorated and the patient developed the clinical criteria of brain death. The patient showed complete areflexia of the cranial nerves and no signs of integrated spinal motor function. The EEG was obtained with two systems and was diagnosed as isoelectric. No components of BAEP could be recorded (Fig. 3).
Figure 3
At the same time TCD showed residual perfusion in the right and left middle cerebral arteries (Fig. 4).
Figure 4
EEGs were obtained twice daily with two systems and were consistently isoelectric. Perfusion was still present 4 days after the development of the isoelectric EEG. The clinical status was unchanged and consistent with brain death.
MR angiography was performed to evaluate herniation of the brain stem and cerebellum in the foramen magnum due to traumatic intracerebral bleeding (Fig. 5). The intracranial segment of the basilar artery could not be imaged. The intracranial segment of the left vertebral artery was narrow. The right vertebral artery could not be imaged. The intracranial segments of both internal carotid arteries were seen in the carotid syphon and after passage of the sinus cavernosus on both sides to the origin of the middle cerebral arteries. Both middle cerebral arteries were seen to be narrowed in the proximal segments (M1) and were not imaged further peripherally.
The EEG recorded with the active cable electrode 4 days after the first conventional isoelectric EEG is shown in Fig. 6. The active cable EEGs showed residual bioelectric activity for 4 days, during which the conventional EEGs remained isoelectric until the flow patterns of both middle cerebral arteries became systolic spikes. The steady decline of the flow profiles is shown in Fig. 7.
Figure 6
Discussion
Determination of irreversible cessation of all cerebral function is based mainly on the clinical status. Additional widely used tests include neurophysiologic and neurovascular tests such as the EEG, evoked potentials (1,9), stimulus-induced 40-Hz oscillations (5), TCD (10), and angiographic techniques.
Various professional societies have formulated guidelines for EEG recording techniques in the evaluation of brain death. For example, the German Society for Clinical Neurophysiology recommends that the noise level of the EEG apparatus should be low enough that EEG potentials can be accurately discriminated from an isoelectric EEG at a level of 2 µV.
The active cable electrode EEG system can measure biosignals in very small dimensions and can record bioelectric brain activity with few artifacts. It can record bioelectric signals that cannot be picked up by conventional techniques. EEG registrations by the active cable electrode showed clear residual bioelectric activity in a patient with severe head injury in whom conventional EEGs with two system showed isoelectric recordings. Simultaneously, TCD showed residual perfusion in both middle cerebral arteries.
Brain death marks human death in the scientific medical sense. Brain death can be determined in any critical care unit on the basis of clinical findings only, without further testing. Our findings suggest that if additional testing is performed — and more tests and more sophisticated and sensitive tests are likely — we will have to deal with the concept of relative, currently technically feasible precision. The documentation of irreversible cessation of all cerebral function on the basis of tests should be based on up-to-date medical and scientific equipment and procedures.