Monitoring and Prevention of Awareness in Trauma Anesthesia
V Borzova, C Smith
Citation
V Borzova, C Smith. Monitoring and Prevention of Awareness in Trauma Anesthesia. The Internet Journal of Anesthesiology. 2009 Volume 23 Number 2.
Abstract
Objectives
-
Review the incidence of awareness in trauma
-
Discuss the risk factors and consequences of awareness in trauma
-
Formulate a rational plan for prevention of awareness in trauma
-
Review the management of awareness during anesthesia
Introduction
Intraoperative awareness is defined as patient's consciousness during a procedure performed under general anesthesia with subsequent recall of the events. 1 Awareness during general anesthesia has received increased attention among the medical profession and lay public in recent years. The Joint Commission on Accreditation of Healthcare Organizations issued a Sentinel Event Alert in 2004 aimed at reducing the risks and managing the impact of anesthesia awareness. 2 Introduction of technologies capable of quantifying the depth of anesthesia, most notably the Bispectral Index monitor (BIS), has given clinicians additional tools to monitor intraoperative levels of consciousness. Prospective, randomized multicenter studies looking at the incidence of intraoperative awareness 3 and use of BIS monitoring as a way to prevent it, 4 5 have been conducted. The American Society of Anesthesiologists (ASA) incorporated the results of these and additional studies and developed a Practice Advisory for Intraoperative Awareness and Brain Function Monitoring to assist anesthesiologists in minimizing the risks of awareness under general anesthesia. 6 The Practice Advisory acknowledged that certain patient characteristics (substance use or abuse, limited hemodynamic reserve, ASA physical status 4 or 5), certain surgical procedures (trauma and cardiac surgery, Cesarean delivery) as well as anesthetic techniques (rapid sequence induction, reduced anesthetic doses especially in the presence of paralysis) place patients at increased risk of intraoperative awareness. The purpose of this article is to review the Practice Advisory and other available literature with special emphasis on monitoring and prevention of awareness in trauma patients.
Incidence
The incidence of intraoperative awareness is estimated to be 0.1-0.2% in the general surgical population (Table 1). 7
Cardiac surgery and Cesarean deliveries have a higher incidence of recall 8 9 with awareness as high as 11-43% reported in major trauma patients. 10 However, in a 1999 study of 96 trauma patients, only one patient had auditory recall. 11 In a prospective, nonrandomized multicenter study of 19,575 patients, a total of 25 awareness cases were identified (0.13% incidence). 12 There were 46 additional cases (0.24%) of possible awareness and 1183 cases (6.04%) of possible intraoperative dreaming. 16 Awareness accounted for 2% of 1,977 general anesthesia claims from 1990 to 2001 including 56 claims for recall and 9 claims for awake paralysis. 13 A median payment of $34,049 (United States $) was made in 52 percent of recall claims. Interestingly, there were no reports of awareness in trauma claims. 14 This discrepancy may be due to improvements in trauma resuscitation, thus permitting the administration of adequate doses of anesthetic agents to trauma patients. 15
Consequences
Awareness is a serious complication of anesthesia. It is often described by patients as their worst hospital experience. 11 Patients report paralysis, pain, perception of surgical manipulations and ability to hear conversations. Auditory perception and the sensation of paralysis are the most frequently reported sequelae, followed by the sensation of pain. 15 Feelings of panic, helplessness and pain are not uncommon. Some patients may develop post-traumatic stress disorder. Psychiatric complications are more likely if pain accompanies the awareness. 16 However, as noticed in Practice Advisory, “in some circumstances, intraoperative awareness may be unavoidable to achieve other critically important anesthetic goals”. 1
Etiology And Risk Factors
In a prospective, open, cross-sectional study of the incidence of awareness in 2612 elective surgery patients, the doses of isoflurane and propofol were significantly lower in patients with awareness. 8 (Table 2) In the study, a large proportion of the patients with awareness were found to have a history of major depression and also had preoperative symptoms of depression and anxiety. 8 Female gender and anesthetic techniques using intraoperative opioid and neuromuscular blocking agents without a volatile anesthetic was associated with a higher frequency of malpractice claims for awareness in the ASA Closed Claims Project. 17 Accidental paralysis of patients prior to induction of anesthesia due to intravenous infusion errors involving succinylcholine drips or syringe swaps when a muscle relaxant was injected instead of a sedative, opioid or hypnotic agent is a common cause of awake paralysis. 18 In a multicenter US trial, (Table 3) awareness was associated with increased ASA physical status (odds ratio, 2.41; 95% confidence interval, 1.04–5.60 for ASA status III–V compared with ASA status I–II). 3 Age and gender did not influence the incidence of awareness.
The presence of conditions that may decrease anesthetic requirement such as hypotension, hypothermia, acidemia, alcohol intoxication, and severe anemia did not reliably prevent awareness during surgery for major trauma when the primary anesthetic agent was discontinued for 20-80 min in 6 severely injured patients. 14 However, 1 patient with a body temperature of 30.5 o C did not suffer awareness during surgery despite the absence of any anesthetic agent for over 4 hours. 14
The ASA Practice Advisory proposed a systematic approach for monitoring and prevention of intraoperative awareness. 1 It recommends the identification of risk factors associated with intraoperative awareness (Table 4, Fig 1).
Figure 4
Causes and consequences of awareness. FROM Ghoneim MM: Awareness during anesthesia. Anesthesiology 2000;92:597-602. Figure 1 on page 598. [PUBLISHER TO OBTAIN PERMISSION]
Patients identified to be at risk for intraoperative awareness should be informed of their risks. 19 The most frequent identifiable cause of awareness during general anesthesia is low or no concentrations of the primary anesthetic agent. Therefore, anesthesia providers should adhere to the checklist protocol for anesthesia machines and equipment to assure that the desired anesthetic drugs and doses will be delivered. The proper functioning of intravenous access, infusion pumps, and their connections, including the presence of appropriate backflow check valves should be insured. Care should be taken to avoid accidental paralysis prior to induction due to infusion errors or syringe swaps involving paralytic medications. Midazolam was noticed to be associated with lower frequency of intraoperative awareness in one double -blinded randomized clinical trial. 20 The decision to administer benzodiazepines or scopolamine prophylactically should be made on case-by-case basis for selected patients. Benzodiazepines and scopolamine can also be administered intraoperatively in an effort to prevent awareness if a patient wakes up unexpectedly during surgery.
Prevention Of Awareness
The problem with awareness during general anesthesia is that the recall component can only be detected postoperatively by interviewing the patient. The question is whether monitoring the anesthetic depth will prevent awareness and what tools do we have to monitor the anesthetic depth. Clinical signs such as purposeful or reflex movement, response to commands, eyelash reflex, pupillary diameters, perspirations, and tearing are valuable but not reliable measures of anesthetic depth. Standard ASA monitoring assessing blood pressure, heart rate, respiratory rate and end-tidal anesthetic concentrations should be used routinely, but also lack specificity. There are reports of awareness in the absence of elevated blood pressure and heart rate. 11,21 Use of neuromuscular blocking agents and cardiovascular medications such as beta-blockers can mask somatic and autonomic signs of the depth of anesthesia. (Table 5)
Figure 6
Concentration-effect relations of inhalational agents provide a guide to the depth of anesthesia. Minimal values of 0.8-1.0 MAC of volatile anesthetics almost always prevent awareness. 21 However, different physiological conditions (aging, substance abuse, pregnancy, hypoxemia, anemia) and individual variability in anesthetic requirements can affect the minimal values of volatile agent or plasma concentration of intravenous anesthetics necessary to prevent recall. Confounding variables that affect the minimal values of volatile agent or plasma concentration of intravenous anesthetic to prevent recall include gender, age, and the arousing effect of surgery and emotionally charged material. 19,23,25 The synergistic effect of drugs such as benzodiazepines, opioids, scopolamine, and other anesthetics with the volatile agents is difficult to quantify because of their varying effects and sites of action. In the 1984 and 1999 studies of awareness in trauma, the standard anesthetic protocol specifically excluded the use of benzodiazepines and scopolamine. 14,15
Brain Function Monitors
Monitoring the state of hypnosis during general anesthesia using commercially available technology has become possible since the introduction of the Bispectral Index (BIS) in 1996. 22 More recently, a number of other brain function monitors processing either spontaneous (Cerebral State Monitor, Entropy, Narcotrend, Patient State Index- Sedline, SNAP) or auditory evoked electrical activity (AEP Monitor/2 ) have been introduced and marketed for assessment of depth of anesthesia. Anesthetic drugs induce dose dependent changes in the electroencephalogram (EEG). (Table 6)
The BIS measures depth of anesthesia by analyzing the EEG to generate a score or index from 0 to 100. 23 The index was derived utilizing a composite of multiple advanced EEG signal processing techniques including bispectral analysis, power spectral analysis, and time domain analysis. (Figs 2 and 3)
.
EEG changes with increasing doses of anesthesia include increased amplitude and decreased frequency. Note the transition from small amplitude, fast frequency in the awake state (BIS = 90-100) to large amplitude, slow frequency with general anesthesia (BIS < 60). From Kelley S: Monitoring consciousness using the bispectral index during anesthesia. A pocket guide for clinicians. Second edition. Reproduced with permission from Dr Kelley, Aspect Medical Systems.
Analysis of a typical EEG segment. Processed EEG parameters of anesthetic effects are 95% spectral edge frequency, median frequency, and relative delta power. Reproduced with permission from Dr Kelley, Aspect Medical Systems, reference 27
The index represents the progression of consciousness from being awake (Index = 100) to no brain activity or isoelectric EEG with BIS value of 0. (Fig 4)
.
Signal processing used for BIS. EEG epochs are digitized and analyzed to look for key EEG features using 3 primary paths: 1. power spectral analysis, 2. bispectral analysis, and 3. time-based analysis. A scaled value is generated based on statistical modeling. There are 4 key EEG features to characterize anesthetic effect: 1. degree of beta frequency activation, 2. amount of low frequency synchronization, 3. presence of nearly suppressed periods within the EEG, and 4. presence of isoelectric periods within the EEG. Reproduced with permission from Dr Kelley, Aspect Medical Systems , reference 27.
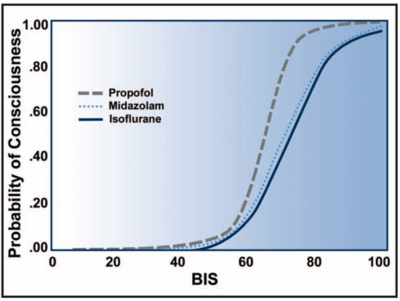
A BIS value between 40-60 is considered suitable for surgical anesthesia and reflects a decreased cerebral metabolic rate and a low probability of consciousness. 24 (Fig 5 and 6)
.
The BIS index reflects reduced cerebral metabolic rate produced by most anesthetics. Using PET scanning, there was a significant correlation between BIS and decreasing brain metabolic activity as measured by glucose metabolism. Reproduced with permission from Dr Kelley, Aspect Medical Systems , reference 27.
.
Logistic regression of probability of consciousness versus BIS for propofol, midazolam, and isoflurane. As BIS decreases below 70, the probability of explicit recall decreases. With BIS < 60, there is an extremely low probability of consciousness. Reproduced with permission from Dr Kelley, Aspect Medical Systems, Kelley SD. Reference 27 [modified from Glass, reference 28]
The cerebral state monitor is a small handheld EEG monitor for determining depth of anesthesia. The entropy monitor measures the degree of entropy, or disorder, in the EEG. Entropy falls with increasing concentration of anesthetic. Entropy calculated in the frequency domain is the basis for the commercially available Entropy monitor which computes 2 parameters- state entropy and response entropy and their difference. 25 State entropy is calculated in the frequency band dominated by the EEG signal (0.8-32 Hz, hypnotic component of anesthesia), whereas response entropy is calculated from 0.8 to 47 Hz (extended frequency response dominated by EMG activity). The Sedline uses derived quantitative 4 channel EEG as a function of hypnotic state to give a patient state index. 26 (Fig 7 and 8)
Primary steps in the development of the patient state index algorithm (Sedline) required the use of 3 databases: 1. normal EEGs and artifacts, 2. EEGs during general anesthesia with a variety of agents, and 3. EEGs in healthy volunteers during general anesthesia with stepwise increases and decreases anesthetic concentration. FROM Drover DD, Lemmens HJ, Pierce ET, et al:Patient state index. Titration of delivery and recovery from propofol, alfentanil, and nitrous oxide anesthesia. Anesthesiology 2002;97:82-9. [PUBLISHER TO OBTAIN PERMISSION] figure 2 on page 87
EEG processing with the patient state index (Sedline). EEG recordings are collected from 2 anterior, a midline central, and a midline posterior scalp location. Artifacts are detected and rejected. EEG data is frequency transformed into subbands and total power. The patient state index is generated as a numeric value from 0 to 100. FROM Drover DD, Lemmens HJ, Pierce ET, et al: Patient state index. Titration of delivery and recovery from propofol, alfentanil, and nitrous oxide anesthesia. Anesthesiology 2002;97:82-9 [PUBLISHER TO OBTAIN PERMISSION] . figure 3 on page 88
The patient state index is based on EEG power, frequency, and phase information from anterior-posterior relationships of the brain, as well as coherence between bilateral regions of the brain. Compared with single channel monitoring, the Sedline provides more information with greater capacity for detecting subtle changes in brain function including density spectral array and raw real-time 4-channel EEG data. The AEP Monitor/2 uses auditory event potentials together with EEG extraction to monitor level of consciousness. Auditory evoked responses have previously been shown to correlate well with level of consciousness and BIS. 27 With the AEP Monitor/2, acoustic stimulation is provided and the evoked response is measured. (Fig 9)
Auditory evoked potential (AEP) response. The brainstem response waves (BAEP) occur within the first 10 ms after the click stimulus. These responses are relative insensitive to general anesthetics. The middle latency waves (MLAEP) occur 10 to 80 ms after the click stimulus – the AAI Monitor extracts the middle latency auditory potentials in the 20 – 80 ms window. They show graded changes with general anesthetics over the clinical concentration range. The late cortical changes (LLAEP) occur 80 ms after the click stimulus and later. These potentials disappear at sedative concentrations of general anesthetics. From: AEP Monitor / 2 Directions for Use for Version 1.6. Danmeter A/S, Kildemosevej 13, DK-5000, Odense C, Denmark. Reproduced with permission from Danmeter A/S
Brainstem response waves occur within the first 10 ms after the click stimulus. These responses are relatively insensitive to general anesthetics. The middle latency waves (early cortical response) occur 10 to 80 ms after the click stimulus. The monitor extracts the middle latency response in the 20 – 80 ms window. They show graded changes with general anesthetics over the clinical anesthetic concentration range. The late cortical changes occur 80 ms after the click stimulus and later. These potentials disappear at sedative concentrations of general anesthetics. An index in the range of 100 – 0 is calculated. (Fig 10)
The AAI index of the AEP Monitor. The AAI index is calculated in the 20-80 ms window of the auditory evoked potential (middle latency AEP) since the brainstem and long latency AEPs do not correlate well with level of consciousness. Latency and amplitude changes in the MLAEP are weighted equally. The AAI is a linear combination of contributions from the MLAEP and EEG. The recommended AAI values for surgical anesthesia are 15-25. From: AEP Monitor / 2 Directions for Use for Version 1.6. Danmeter A/S, Kildemosevej 13, DK-5000, Odense C, Denmark. Reproduced with permission from Danmeter A/S.
In clinical trials, only use of the BIS monitor was associated with decreased awareness. 4,5 The B-aware prospective, randomized, double-blinded, multicenter trial of 2,503 high-awareness risk patients (trauma, cardiac surgery, rigid bronchoscopy, Cesarean delivery) revealed that BIS -guided anesthesia reduced the incidence of awareness with recall by 82%. 4 In another study, routine use of BIS monitoring decreased the incidence of awareness in general surgical patients by 77% comparing to historical controls. 5 In both studies, two patients experienced awareness despite using BIS. Interestingly, all four patients recalled events during periods of significant stimulation (sternal split, tracheal intubation) when BIS values were near or greater than 60. Thus, periods of intense stimulation should be watched carefully and interventions should be undertaken promptly to prevent awareness. In a subsequent meta-analysis of 20 studies with 4056 participants, the authors concluded that BIS guided anesthesia reduced the incidence of intraoperative awareness with recall in surgical patients at high risk of awareness (odds ratio 0.20, 95% confidence interval 0.05 to 0.79). 28
BIS monitoring was used by Lubke et al in acute trauma patients undergoing general anesthesia (etomidate induction, isoflurane and fentanyl maintenance) to determine whether the probability of memory declines with increasing depth of the hypnotic state. 15 These authors found that auditory information processing (implicit memory) occurred at BIS levels between 40 and 60. There was one instance of auditory recall at these levels of general anesthesia. 15
One of the limitations of brain function monitors is that the numerical index can be influenced by different factors. Pacemakers and forced-air warmers among other medical devices can increase BIS values by producing an electromechanical artifact. 27 Ketamine may increase BIS due to its unique pattern of EEG activation. 29 Transient paradoxical response to increased isoflurane concentration has been reported. 30 Excessive muscle tone from forehead muscles may increase BIS and is known as electromyographic (EMG) artifact. Neuromuscular blocking agents can alleviate EMG artifact and result in decreased BIS. Rapid changes in BIS values were reported with cerebral ischemia, gas embolism, unrecognized hemorrhage, and hypoglycemia (Figure 11). 31
Fig 11. Influence of artifacts (electromagnetic- EMG, electromechanical) and reduced cerebral metabolism (cardiac arrest, hypoperfusion, hypothermia) on bispectral index. From Kelley S: Monitoring consciousness using the bispectral index during anesthesia. A pocket guide for clinicians. Second edition. Reproduced with permission from from Dr Kelley, Aspect Medical Systems.
Preexisting patient conditions can influence BIS values as reported in a volunteer with genetically determined low-voltage EEG signals. 32 BIS values should be interpreted with caution in patients with neurological disorders. Despite these limitation, monitoring BIS provides a better measure of the hypnotic state compared with autonomic responses and better measure of pharmacodynamic effect of an anesthetic agent compared with end-tidal or target plasma concentrations.. 33 Moreover, BIS guided anesthesia has been shown to decrease the incidence of awareness, decrease recovery time (time to eye opening, response to verbal command, extubation and orientation) and shorten duration of postanesthesia care unit stay. 4,5,33
Management Of Awareness
Anesthesia awareness cannot always be prevented. If a patient unexpectedly becomes conscious during the surgery, the practitioner can consider using benzodiazepines and/or scopolamine. 23 However, there are no studies that evaluated efficacy of this approach in reducing the occurrence of awareness. Once an episode of intraoperative awareness has been reported, practitioners must acknowledge and manage the patient with compassion and diligence. The details of the event should be discussed with the patient as well as possible reasons for its occurrence. (Table 7)
The patient should be assured of credibility of this account. Finally, counseling and psychological support should be offered including referral to a psychiatrist or psychologist. 20,23 Pain, anxiety and delayed neurotic symptoms were more common if awareness occurred in conjunction with neuromuscular blockade. 7 The delayed neurotic symptoms resolved within 3 weeks in all patients after repeated discussion and information. 7 Future studies are needed to examine the impact of these interventions on patient’s well-being.
Summary And Conclusions
In summary, intraoperative awareness is a serious problem affecting 0.1-0.2% of the general surgical population. Patients at high risk of awareness, such as those with hypotension or limited cardiovascular reserve should be identified preoperatively and informed of the risk, if possible. Steps to ensure the proper delivery of anesthetics should be undertaken. Multiple modalities including standard ASA monitors and clinical observations of reflexes and movements in nonparalyzed patients should be routinely employed. Use of complete neuromuscular blockade should be avoided when possible. The decision to use benzodiazepines, scopolamine and BIS monitoring should be made on case-by-case basis in selected patients. We feel that brain function monitoring such as BIS should be routine in high risk surgical patient populations such as previous episode of awareness, patients with limited hemodynamic reserve, cardiac surgery, reduced anesthetic doses during paralysis, and somatosensory or evoked potential monitoring. If intraoperative awareness is reported postoperatively, patients should be offered support and psychological counseling.