Interpersonal and Cross Cultural Communication for Advance Practice Registered Nurse Leaders
A Boykins, C Carter
Keywords
advance practice registered nurses, communication, culture, health care provider, nurse leaders
Citation
A Boykins, C Carter. Interpersonal and Cross Cultural Communication for Advance Practice Registered Nurse Leaders. The Internet Journal of Advanced Nursing Practice. 2012 Volume 11 Number 2.
Abstract
Advance practice registered nurse (APRN) leaders require advanced level communication skills in order to provide safe and effective care. Knowledge and skills in interpersonal and cross cultural communication are important for the APRN when providing care to patients and when working in interprofessional teams. This article will discuss the application of professional standards of culturally competent care and communication in the APRN provider-patient interaction and the APRN leadership role at the organizational level. Cross cultural communication and leadership knowledge and skills are essential for APRN leaders in meeting the cultural and language needs of patients and delivery of culturally appropriate and competent care.
Introduction
Communication is a cultural phenomenon that affects nursing care among cultural groups.1 Since nurses are the largest group in the United States (US) health care workforce, nurses are best positioned to champion holistic care that recognizes an individual’s preferences, values and needs, and respects the patient or designee as a full partner in providing compassionate and culturally appropriate, safe and effective care.2 The Institute of Medicine provided a blueprint for the future of nursing across roles, settings and educational levels, and addressed how the work environment of nurses can be transformed to keep patients safe.2,3 The advance practice registered nurse (APRN) is one of many nursing roles.
Advanced level communication skills including effective communication between patients, nurses, and other clinical leaders are essential to ensuring safe and reliable care.2, 3 Communication is also a vital component of culturally competent care provided by APRN health care providers and leaders. The APRN has to address individual and cultural differences when communicating with patients, and the APRN leader should also possess advanced level interpersonal and cross cultural communication skills in order to communicate effectively and provide culturally appropriate, safe, effective, and quality care to patients. More importantly, the APRN has to be willing to develop a therapeutic relationship with someone that is culturally different and also recognize that differences in communication style may affect the therapeutic relationship. In addition to establishing a therapeutic relationship with someone that is culturally different, the APRN is expected to negotiate patient-centered, culturally appropriate, and evidence-based goals and treatment plans with the patient.4 The APRN has to understand how culture impacts communication in the nurse-patient relationship and consider the patient’s cultural and language needs when communicating with the patient and developing a plan of care. This article will discuss application of professional standards of culturally competent care and communication in the APRN provider-patient interaction and the APRN leadership role at the organizational level.
Interpersonal Communication Skills
Communication is a process of exchanging information between a source and recipient, has to be mutually understandable, and requires language skills. Language is used as a tool to exchange and understand information. The use (linguistics), structure (syntactic), and meaning (semantics) of language are important in the communication process. The overall purpose of semantics is alleviating misunderstanding when communicating. Furthermore, common meaning, understanding or clarity in communication is necessary for effective communication. Effective communication occurs when APRN health care providers understand and integrate the information obtained from patients, and when patients understand accurate, timely, complete, and clear messages from APRNs so that they can participate responsibly in their care. The APRN health care provider must also communicate effectively with patients’ families and other health care professionals to promote mutual respect and shared decision making.5
Effective communication in nursing is therapeutic and requires interpersonal communication skills. Interpersonal communication skills are part of the therapeutic process that is established between the nurse and the patient. Peplau’s interpersonal relations in nursing theory was developed several decades ago and provided the foundation for the first APRN role and master’s degree nursing program, the psychiatric and mental health clinical nurse specialist and master’s degree in psychiatric nursing. 6, 7 Concepts in Peplau’s theory are the therapeutic nurse-patient relationship, communication (verbal and nonverbal communication), and interpersonal techniques. The concepts are integral to the therapeutic interpersonal process which was designed as a psychotherapeutic approach for nurses to assess and develop a plan to solve a patient’s problems. Knowledge and skills in verbal and nonverbal communication are necessary in the APRN provider-patient interaction in order to assist patients in regaining their health and well-being.7
Verbal communication is the spoken or written word and has private and shared meanings. Denotation is the actual meaning or the general use of the word and connotation is the implied meaning and comes from personal experience. Most communication is nonverbal and involves body language, sounds, voice quality, nonverbal signs, personal and social space, touch, appearance, and cultural artifacts.
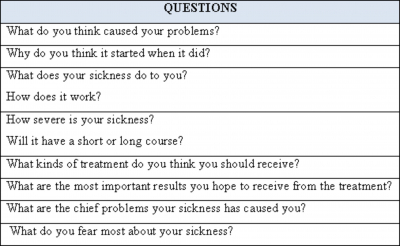
Effective communication and deliberate actions taken by the nurse to achieve therapeutic goals occur in three phases during the APRN provider-patient relationship: orientation, working, and termination or resolution.7, 8 During the orientation phase of the provider-patient relationship, the APRN conducts an assessment and formulates a diagnosis. The assessment requires communication with the patient and interviewing skills. Knowledge about the patient’s culture, beliefs and values and the APRN culture, values, beliefs, and view of self are important to the provider-patient relationship. More important, APRNs should know how to evaluate a patient’s health care concerns that are not documented in the medical record or those concerns that are not communicated by the patient when conducting an assessment. The Patient Explanatory Model is a framework that was also developed several decades ago to examine the meaning of disease and illness among health care providers and patients. 9 Concerns of health care providers are diagnosis and treatment of disease while patients are concerned with the experience of suffering with an illness. Meaningful explanations of illness are important to the patient; therefore, cultural influences such as values, beliefs, personal, and social issues should be considered by health care providers when providing health care. The Patient Explanatory Model can be implemented in the orientation phase of the APRN provider-patient relationship. Use of the Patient Explanatory Model in eliciting the patient’s explanation regarding the cause of the health concern can reveal insights to the psychosocial and cultural meaning of illness and can be enlightening for the APRN in formulating a differential diagnosis. An evaluation of the patient’s concerns regarding illness can be accomplished by asking the patient questions in the Patient Explanatory Model (Table 1). The assessment of both disease and illness problems as well as the patient’s therapeutic goals should be documented in the patient’s medical record.9
The next phase of the nurse-patient relationship is the working phase where a plan is formulated and implemented based on identifying patient outcomes. Open communication with the patient is important so that the patient is intimately involved in executing the plan and in achieving the goals and outcomes of the plan of care. Mutual respect between the patient and provider is accomplished by asking the patient if certain health interventions planned are mutually agreeable and more importantly, obtain permission from the patient before proceeding with care. Issues are resolved, discharge or follow-up instructions are provided, and a plan to maintain health is provided during the last phase, the resolution or termination phase. The patient has to successfully transition through all of the phases of the nurse-patient relationship, and the APRN assumes many roles (stranger, resource person, teacher, leader, surrogate, and counselor) when communicating with the patient during each phase.7, 8
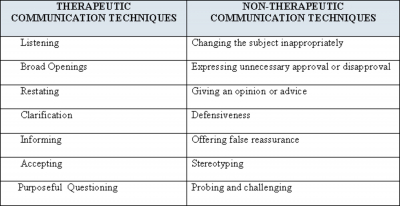
The therapeutic interpersonal process looks at other influences associated with the patient’s problem, and interpersonal techniques are used throughout the phases of the provider- patient relationship.8 The APRN has to possess qualities of mutual respect, compassion, trust, and empathy when using interpersonal techniques. Other interpersonal techniques and responsive skills to facilitate therapeutic communication are genuineness and concreteness. Therapeutic and nontherapeutic communication techniques that a nurse may use when communicating with a client are listed in Table 2. Listening is one of the foundational interpersonal communication techniques and is equally important in cross cultural communication. Listening shows interest in and respect and acceptance of the patient. Although APRNS have the knowledge and skills necessary to manage the care of their patients, interpersonal communication techniques including listening requires concentration. In the interpersonal therapeutic process, a therapeutic environment is created by the APRN, and the patient and APRN have a supportive and collaborative relationship. Effective communication using interpersonal communication techniques is an essential requirement of the provider-patient relationship and is necessary prior to acquiring effective cross cultural communication skills.
Cross-Cultural Communication Skills
Nursing has identified 12 standards for cultural competence in direct clinical practice, research, education, and administration. Two of the 12 standards are cross cultural communication and cross cultural leadership. The term, cross-cultural is defined in the Standards for Culturally Competent Nursing Care as “any form of activity between members of different cultural groups”.10(p. 24) Standard 9: Cross-Cultural Communication states that “nurses shall use culturally competent verbal and nonverbal communication skills to identify client’s values, beliefs, practices, perceptions, and unique health care needs”.10 (p.17) Standard 10: Cross-Cultural Leadership states that “nurses shall have the ability to influence individuals, groups and systems to achieve positive outcomes of culturally competent care for diverse populations”.10 (p. 19)
In order to identify patients’ values, beliefs, practices, perceptions, and unique health care needs when communicating cross culturally, the APRN has to develop cultural awareness and responsiveness. Cultural awareness “is being knowledgeable about one’s own thoughts, feelings, and sensations and having an appreciation of the diversity of others”.11(p.100) The culturally responsive APRN has to self-reflect on his/her own cultural identity, personal beliefs, language, norms, and behaviors to determine how they guide his/her perceptions and interactions with the patient. Respectful and reciprocal communication with the patient regardless of differences with the patient is necessary. The APRN has to be culturally responsive or aware that the patient’s beliefs, language, norms, and behaviors are learned and shared and guide the patient’s thinking, decisions, and actions. Consequently, the patient’s culture not only shapes the meaning of the individual’s behavior but also that person’s health-seeking and health-related behaviors.
The APRN also implements patient-centered and culturally responsive strategies in the delivery of clinical prevention and health promotion interventions and/or services to individuals, families, communities, and aggregates/clinical populations.12 The APRN has to value and accommodate for the different styles of communication used by patients, families, and other health care professionals and identify cultural barriers to effective communication.13 Cross cultural communication barriers have been addressed by the IOM3 and in the standards of professional nursing practice.13 Personal and psychosocial obstacles that may exist for the patient and affect cross cultural communication are lack of English language proficiency, limited vocabulary, inaccurate pronunciation, and not being familiar with slang or regional dialects. Additionally, provider-patient barriers other than language that may exist are racial and ethnic concordance between the patient and provider and the provider’s cultural competency.14
Cultural competence is “having the capacity to function effectively as an individual and an organization within the context of the cultural beliefs, behaviors and needs presented by consumers and their communities”.15 (p.131) Nursing models that exist for developing cultural competence include4:
Mnemonics can be used when communicating during the three phases of the APRN provider-patient relationship. In addition to developing cultural competence, responsiveness, and awareness, the nurse has to obtain cultural knowledge about the diverse cultural and ethnic groups and patient’s health-related beliefs and values and world views.24
Cross Cultural Communication in the APRN Provider-Patient Interaction
APRN health care providers should provide care and services that are equitable and responsive to the unique cultural and ethnic identity, socio-economic condition, emotional and spiritual needs, and values of patients and populations.25, 26 For example, socio-economic conditions that may exist are related to poverty, access to care, quality care, social position, sexual orientation, immigration status, and educational level. Emotional needs may include mental health problems and psychiatric diagnosis. The APRN role encompasses reducing and /or eliminating health disparities and addresses individual and cultural differences including communication.
Giger and Davidhizar’s Transcultural Assessment Model delineates six areas of human diversity and differences evident in all cultural groups. 1 One of the areas of human diversity and differences is communication and factors that influence communication are universal, but vary among culture-specific groups in terms of language spoken, use of silence, and use of verbal and nonverbal communication. Attributes of nonverbal and verbal communication are warmth and humor.1 Additionally, the cross cultural communication standard for cultural competence in nursing practice states that nurses shall use culturally competent verbal and nonverbal communication skills to identify client’s values, beliefs, practices, perceptions, and unique health care needs.10 The APRN needs to be aware of culturally specific verbal communication used by the patient such as voice volume, quality, tone, intonation, rhythm, and speed; reflections; vocabulary; pronunciation; grammatical structure; and willingness to share thoughts and feelings. Thoughts and feelings about the cause of the illness and beliefs about what treatments will make the patient better should be determined. An assessment should also be conducted on the use of formal and informal language in the patient’s culture. For example, different dialects are used within cultures and may be related to geographical location. Differences in dialect and formal greetings also exist in different areas of the US. For example, endearing terms such as “honey, baby, sweetie, darling, and sugar” are appropriate greeting terms in certain areas of the US, but may be considered demeaning by some patients. Likewise, when greeting someone in the US and other western cultures, an individual’s first name comes before the family name; therefore, the patient will be greeted by their family name. On the other hand, the family name precedes the first name in some eastern cultures and greeting the patient by the first name would not be correct. The APRN should determine the patient’s preference for addressing him/her by name.
Nonverbal communication can be due to sociocultural norms and may be expressed in body language such as body motions, reflexes, touch, facial expressions, eye contact, gestures, posture, appearance and cultural artifacts. Nonverbal sounds that the patient may exhibit are groaning, grunting, laughing, and crying. Grooming and hygiene are reflected in the appearance of the patient.7 Cultural artifacts may include clothes, cosmetics or makeup, perfume, and jewelry. The APRN has to confirm with the patient the meaning and significance of cultural artifacts in nonverbal communication and provide culturally appropriate nonverbal communication. One way to help bridge cross cultural communication gaps is to learn how to effectively read the body language of patients. In many instances, nonverbal communication by patients tell APRNs more than could or would be verbally communicated. For example, in some cultures females are not allowed to speak with or question a man that is not in her family which may pose a problem with communication if a male APRN is providing care to the female. Gestures such as shaking the head, pointing fingers or using a thumb up sign is not recognized or not appropriate among some cultural groups. Additionally, greeting a patient with a handshake is also not appropriate in some cultures. Examples of culturally specific verbal and nonverbal communication are listed in Table 4.1,10
In summary, cross cultural communication skills are culturally congruent measures to improve the effectiveness of communication. As health care providers, APRNs should recognize how individuality contributes to effective communication, conflict resolution, and positive interprofessional working relationships. In some cultures, conflict is avoided; therefore, some patients may not understand or agree with the APRN and will not respond. Conflict can occur in ineffective communication; therefore, the APRN leader must recognize that effective communication is a process and requires commitment, practice, and continuous improvement in communication and conflict resolution skills.13 Likewise, the APRN and other providers who work in interprofessional teams need to be aware of patient’s values, preferences, and cultural values for decision making and management of their care.26
The APRN Cross Cultural Leader
Advanced practice registered nurse leaders must possess the knowledge, skills, and attitude to be competent in cross cultural communication. In other words, the APRN will use culturally competent verbal and nonverbal communication skills in order to identify client’s values, beliefs, practices, perceptions, and unique healthcare needs.10 Additionally, the APRN leader can promote a professional environment that includes accountability and advanced level communication skills and is able to use effective communication strategies to develop, participate, and lead interprofessional teams.12 The APRN leader can assume the leadership role in interprofessional teams by implementing patient safety and quality improvement initiatives using effective public communication through professional writing and speaking as well as group interactions. Group interactions include the relationship between the nurse and patient and relationships between nurses and other health care providers, as well as nurses and administrators. APRNS should also function as leaders in redesigning health care.2 For example, APRN nurse leaders need to take proper precautions to avoid cultural gaffes. A gaffe is defined as a social blunder or faux pas. Observing the demographics of the patients that frequent the health care setting for care is one way to avoid cultural gaffes. Seeking knowledge on the cultural norms of the cultural group heavily represented in the health care setting will prevent cultural gaffes. Cross cultural leadership includes influencing individuals, groups, and systems to achieve culturally competent care with positive outcomes for diverse populations. The APRN leader seeks continuous cultural competence through self-development and by encouraging cultural competence development of other members of the interprofessional team.10,13 A cultural competence health practitioner assessment, The Cultural Competence Health Practitioner Assessment (CCHPA), exists so that health care providers can assess their cultural competence. The assessment consists of 6 subscales and 1 of the scales is cross-cultural communication.27
The National Standards on Culturally and Linguistically Appropriate Services (CLAS) are standards for health care providers and health care organizations to make their practices more culturally and linguistically accessible. The 14 standards are organized by themes: Culturally Competent Care (Standards 1-3), Language Access Services (Standards 4-7), and Organizational Supports for Cultural Competence (Standards 8-14). Nurses and APRN providers can complete free online educational training associated with the 14 standards.28
In partnership with other health care professionals, the APRN is expected to take a leadership role in eliminating health disparities and addressing globalization. The APRN leader’s role in education, research, policy, and practice incorporates advocating for patients and policies that advance health care, addressing social justice, understanding complex causes of health disparities, and modifying attitude and personal transformation. An additional APRN leader role is investigating and/or understanding the effects and contribution of socio-cultural factors in healthcare services outcomes. The APRN leader can develop, implement, and evaluate culturally competent care by ensuring that appropriate cross-cultural communication occurs in all health care settings for patients with limited English proficiency, health literacy problems, and/or nonverbal communication.13 In addition to being culturally competent, APRN leaders need to develop linguistic competency. Linguistic competency is defined as:
The APRN has to not only consider the needs of individuals from different cultures but also the needs of individuals that speak a language other than English. Both spoken and written language should be assessed by the APRN and communication provided in the mode of communication preferred by the patient. Linguistic competency requires health care professionals and organizations to respond effectively to the health literacy needs of patients served including policies, structures, practices, procedures, and dedicated resources to support linguistic competency.29 Organizations should have language access services including interpreters, telephone access services, and translated written materials to address the needs of linguistic minorities.
More importantly, the APRN leader has to create an environment of cultural competence. When working with interprofessional teams, the APRN leader has to recognize qualities unique to individual members of the interprofessional team. Unique interprofessional team qualities are experience level, area of expertise, culture, power, and hierarchy within the team.30 The APRN leader fosters an open communication environment among members of the interprofessional team and recognizes the cultural diversity of team members. Each team member contributes to the communication norms of the team and healthy learning, and conflict resolution is encouraged. For example, the APRN leader may need to confront another member of the team if a cultural gaffe or social blunder has been committed against a team member. Cultural mishaps are learning opportunities for the interprofessional team. Learning opportunities may include learning how culture impacts communication and identifying cultural communication barriers. Team huddles, a form of group interaction, is a strategy to deal with cultural mishaps and barriers and provides an opportunity for frequent effective communication and team building. Trust is also established when the APRN leader encourages positive interprofessional working relationships among diverse team members by respecting the individual and cultural differences of team members.30 When communicating with team members from different cultures, the APRN leader has to respect the area of expertise and experience level of team members in meeting the patient’s health care needs as well as accommodate for the different styles of communication. In order for the APRN to become an effective leader, effective interpersonal and cross cultural communication skills are needed to accommodate for the unique cultural qualities among members of the interprofessional team.
Conclusion
The culturally competent APRN leader incorporates the patient’s culture and spiritual preferences, values, and beliefs when communicating with the patient and providing care. Care involves health promotion/disease prevention as well as assessment, diagnosis, and treatment of the patient’s problems. APRNs also have a complexity of other knowledge and skills including interpersonal and cross cultural communication skills. Although culture influences the APRN provider-patient interaction and the APRN leader interaction with other health care providers, APRNs need to recognize that developing cultural competency is a process. In order to reduce or eliminate health care disparities, APRNs have to provide culturally appropriate, culturally competent, and culturally diverse care to cultural and linguistic minorities. Outcomes from interpersonal and cross cultural communication and leadership include improved access to health care, health service coordination and utilization, health outcomes, quality of care, and patient satisfaction.